

Cervical spondylosis is a common degenerative condition of the cervical spine. It is most likely caused by age-related changes in the intervertebral disks. Clinically, several syndromes, both overlapping and distinct, are seen. These include neck and shoulder pain, suboccipital pain and headache, radicular symptoms, and cervical spondylotic myelopathy (CSM). As disk degeneration occurs, mechanical stresses result in osteophytic bars, which form along the ventral aspect of the spinal canal.
Frequently, associated degenerative changes in the facet joints, hypertrophy of the ligamentum flavum, and ossification of the posterior longitudinal ligament occur. All can contribute to impingement on pain-sensitive structures (eg, nerves, spinal cord), thus creating various clinical syndromes. Spondylotic changes are often observed in the aging population. However, only a small percentage of patients with radiographic evidence of cervical spondylosis are symptomatic.
Treatment is usually conservative in nature; the most commonly used treatments are nonsteroidal anti-inflammatory drugs (NSAIDs), physical modalities, and lifestyle modifications. Surgery is occasionally performed. Many of the treatment modalities for cervical spondylosis have not been subjected to rigorous, controlled trials. Surgery is advocated for cervical radiculopathy in patients who have intractable pain, progressive symptoms, or weakness that fails to improve with conservative therapy. Surgical indications for cervical spondylotic myelopathy remain somewhat controversial, but most clinicians recommend operative therapy over conservative therapy for moderate-to-severe myelopathy.
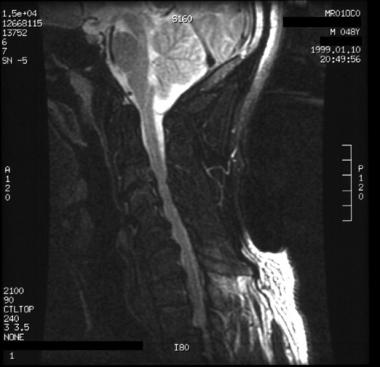 A 48-year-old man presented with neck pain and predominantly left-sided radicular symptoms in the arm. The patient's symptoms resolved with conservative therapy. T2-weighted sagittal MRI shows ventral osteophytosis, most prominent between C4 and C7, with reduction of the ventral cerebrospinal fluid sleeve.
Next
A 48-year-old man presented with neck pain and predominantly left-sided radicular symptoms in the arm. The patient's symptoms resolved with conservative therapy. T2-weighted sagittal MRI shows ventral osteophytosis, most prominent between C4 and C7, with reduction of the ventral cerebrospinal fluid sleeve.
Next
Cervical spondylosis is the result of disk degeneration. As disks age, they fragment, lose water, and collapse. Initially, this starts in the nucleus pulposus. This results in the central annular lamellae buckling inward while the external concentric bands of the annulus fibrosis bulge outward. This causes increased mechanical stress at the cartilaginous end plates at the vertebral body lip.
Subperiosteal bone formation occurs next, forming osteophytic bars that extend along the ventral aspect of the spinal canal and, in some cases, encroach on nervous tissue.[1, 2] These most likely stabilize adjacent vertebrae, which are hypermobile as a result of the lost disk material.[3, 4] In addition, hypertrophy of the uncinate process occurs, often encroaching on the ventrolateral portion of the intervertebral foramina.[1] Nerve root irritation also may occur as intervertebral discal proteoglycans are degraded.[5]
Ossification of the posterior longitudinal ligament, a condition often seen in certain Asian populations, can occur with cervical spondylosis. This condition can be an additional contributing source of severe anterior cord compression.[6]
Cervical spondylotic myelopathy occurs as a result of several important pathophysiological factors. These are static-mechanical, dynamic-mechanical, spinal cord ischemia, and stretch-associated injury. As ventral osteophytes develop, the cervical cord space becomes narrowed; thus, patients with congenitally narrowed spinal canals (10-13 mm) are predisposed to developing cervical spondylotic myelopathy.
Age-related hypertrophy of the ligamentum flavum and thickening of bone may result in further narrowing of the cord space.[2, 7, 8] Additionally, degenerative kyphosis and subluxation are fairly common findings that may further contribute to cord compression in patients with cervical spondylotic myelopathy.[6, 9] Dynamic factors relate to the fact that normal flexion and extension of the cord may aggravate spinal cord damage initiated by static compression of the cord. During flexion, the spinal cord lengthens, resulting in it being stretched over ventral osteophytic bars. During extension, the ligamentum flavum may buckle into the cord, pinching the cord between the ligaments and the anterior osteophytes.[7, 10]
Spinal cord ischemia also most likely plays a role in cervical spondylotic myelopathy. Histopathologic changes seen in persons with cervical spondylotic myelopathy frequently involve gray matter, with minimal white matter involvement—a pattern consistent with ischemic insult. Ischemia most likely occurs at the level of impaired microcirculation.[11]
Stretch-associated injury has recently been implicated as a pathophysiologic factor in cervical spondylotic myelopathy.[12] The narrowing of the spinal canal and abnormal motion seen with cervical spondylotic myelopathy may result in increased strain and shear forces, which can cause localized axonal injury to the cord.
Cervical spondylotic myelopathy is the most common cause of nontraumatic spastic paraparesis and quadriparesis. In one report, 23.6% of patients presenting with nontraumatic myelopathic symptoms had cervical spondylotic myelopathy.[13]
Cervical spondylosis may affect males earlier than females, but this is not true in all studied populations.
Irvine et al defined the prevalence of cervical spondylotic myelopathy using radiographic evidence. In males, the prevalence was 13% in the third decade, increasing to nearly 100% by age 70 years. In females, the prevalence ranged from 5% in the fourth decade to 96% in women older than 70 years. Another study examined patients at autopsy. At age 60 years, half the men and one third of the women had significant disease.[14] A 1992 study noted that spondylotic changes are most common in persons older than 40 years. Eventually, greater than 70% of men and women are affected, but the radiographic changes are more severe in men than in women.[15]
Copyright © www.orthopaedics.win Bone Health All Rights Reserved