

Superior labral (labrum) lesions can cause painful mechanical symptoms and difficulty with overhead activities whether they be athletic or those of daily living. Superior labrum tears were first described by Andrews.[1] In a study that reviewed their experience in 73 throwing athletes, the authors identified tears of the labrum involving the anterosuperior aspect near the origin of the biceps tendon. They attributed this lesion to the biceps tendon being pulled off the labrum as a result of force generated during the throwing motion.
Snyder et al coined the term SLAP (superior labrum, anterior and posterior) lesion to describe a more extensive injury.[2] A SLAP lesion, as described by Snyder, involves a tear of the superior labrum, which starts posteriorly and extends anteriorly to include the anchor of the biceps tendon to the superior labrum. The injuries were subdivided into four types (I-IV). Much as in Andrews' findings, a subset of patients who reported a traction injury were identified. However, the majority of patients related a history of a compressive injury to the shoulder secondary to a fall on an outstretched arm in a flexed and abducted position.
SLAP lesions, as opposed to occult anterior instability, are likely the underlying cause of the so-called dead arm syndrome in throwing athletes. Regardless of whether injuries to the superior labrum biceps complex are secondary to a throwing or nonthrowing etiology, they can be a source of considerable disability for the patient.
These injuries are difficult to diagnose on physical examination because the findings are often nonspecific and demonstrate considerable overlap with those of other etiologies of shoulder pain. Similarly, both nonenhanced magnetic resonance imaging (MRI) and magnetic resonance arthrography have variable accuracy in determining if a SLAP lesion is present. At times, the only definitive way to diagnose a SLAP lesion is with a diagnostic arthroscopy.[3]
Even so, a thorough understanding of the normal anatomy and biomechanics of the superior labral biceps complex, as well as commonly observed normal anatomic variants, is mandatory to ensure appropriate surgical stabilization and to avoid unnecessary repair of the superior labrum.[4]
Initial operative treatment of superior labral (labrum) lesions consisted of debridement only. This therapy is appropriate for type I and type III lesions, as well as for some type IV lesions, in which the biceps anchor is intact. However, in type II and in type IV lesions in which the biceps anchor is unstable, debridement alone yields poor results.
Early attempts at arthroscopic fixation used a metal staple. This technique was discontinued because of concerns for chondral injury as well as the need for a second surgery for staple removal. For similar reasons, techniques involving a metal screw are no longer used. A transglenoid technique similar in concept to a transglenoid technique for a Bankart repair has been described; however, this is technically difficult and has fallen out of favor. Good results were initially reported with use of a bioabsorbable tack.[5] However, complications, including implant breakage with resultant particulate debris and a foreign body reaction, have been reported.
Suture anchors loaded with nonabsorbable suture is the preferred method of fixation.[6]
NextThe glenoid labrum is a triangular fibrocartilaginous structure that serves to deepen the glenoid. Whereas tears of the anteroinferior labrum have long been known to be associated with significant shoulder pathology, it is really only since the advent of shoulder arthroscopy that injuries of the superior labrum have been appreciated as a potential pathologic lesion.
The superior labrum often has a more meniscoid attachment to the glenoid rim compared with the remainder of the labrum and therefore may be more susceptible to both degenerative and traumatic lesions. It also serves as part of the origin of the long head of the biceps. Injuries to the superior labral biceps complex can compromise the biceps anchor. Furthermore, the repetitive tensile force exerted by the biceps on the superior labrum likely contributes to poor healing of superior labral tears.[7] (See the image below.)
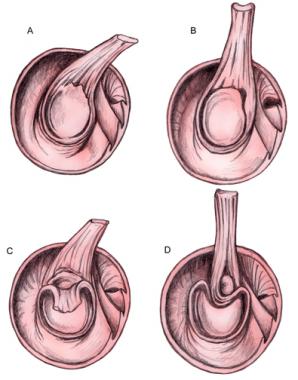 Superior labrum anterior and posterior (SLAP) lesion types.
Superior labrum anterior and posterior (SLAP) lesion types.
Snyder classified superior labral tears into four types as follows[2] :
Modifications have been made to the original classification.
Morgan and Burkhart subdivided the type II lesions into three subtypes: anterior type II, posterior type II, and combined type II (referring to the tear involving the labrum both anterior and posterior to the biceps anchor).[8]
Maffet et al expanded the original classification to include types V, VI, and VII, defined as follows[9] :
Type II lesions are by far the most common and are also the source of the greatest diagnostic difficulty.
To accurately classify superior labral (labrum) lesions, one must be aware of normal anatomy, including the many normal variants that are observed. The biceps tendon origin is divided roughly in half between the supraglenoid tubercle and the superior labrum. Vangsness et al demonstrated that, 55% of the time, the labral insertion is entirely or mostly into the posterior labrum.[10] Only a small percentage (~8%) have a predominant anterior insertion. The remainder have equal insertions to the anterior and posterior labrum.
In an anatomic study, Cooper et al noted that the superior portion of the labrum had a distinctly different morphology from the inferior labrum.[11] The superior and anterosuperior portions were found to be loosely attached to the glenoid rim through thin connective tissue that easily stretched. This is similar to that of the meniscus of the knee. In contrast, the inferior labrum had a firm attachment through thick inelastic fibers and appeared as a firm immobile extension of the glenoid articular cartilage. The 12-o'clock position was the only location on the glenoid rim where the hyaline articular cartilage extended over the rim of the glenoid.
The biceps tendon inserts into the supraglenoid tubercle, which is 5 mm medial to the glenoid rim. This, along with the often meniscoid attachment of the superior labrum, results in a sublabral recess.
This should not be mistaken for a type II SLAP lesion. As reported by DePalma, a sublabral recess may be present in as many as 50% of individuals older than 20 years.[12] This incidence increases with patient age. More than 95% of the specimens in DePalma's study obtained from patients in the seventh and eighth decades of life were found to have a sublabral recess.
The middle glenohumeral ligament can sometimes insert directly into the superior labrum as a large thick cordlike structure (ie, the so-called Buford complex). In these cases, the anterosuperior labrum is absent. The Buford complex is not pathologic and should not be stabilized, because to do so would markedly restrict external rotation. A sublabral foramen can be observed where the anterosuperior labrum, from approximately the 1- to 3-o'clock position in a right shoulder, is loosely attached or not attached at all to the glenoid rim. Again, this is not pathologic and should not be stabilized; to do so would result in a significant loss of external rotation.
Histologically, the superior labrum is composed of fibrocartilage, consisting of type II cartilage in a relatively acellular matrix with occasional interspersed elastin fibrils. This is in contrast to the hyaline cartilage of the glenoid and the dense fibrous glenohumeral capsule. Branches of the suprascapular, circumflex scapular, and posterior humeral circumflex supply the labrum. Periosteal and capsular vessels supply the labrum throughout its periphery. No vessels enter the labrum from the underlying bone. In general, the superior and anterosuperior labrum have less vascularity than other portions of the labrum.
On a biomechanical level, incompetence of the superior labrum and biceps anchor has been shown to have a deleterious effect on anterior glenohumeral stability. In a cadaver study, Rodosky et al compared anterior glenohumeral stability in specimens with an intact superior labrum with those with a SLAP lesion.[13] They demonstrated that the presence of a SLAP lesion decreased the torsional resistance by 11-19%, as compared with the intact shoulder, as it was placed in the abducted and externally rotated position. The inferior glenohumeral ligament was subject to significantly increased strain (increase by >100%) in the presence of a SLAP lesion.
In another cadaver study, Pagnani et al demonstrated that a SLAP lesion results in significant increases in both anterior-posterior and superior-inferior translations.[14] At 45° of elevation, a 6-mm increase was noted in anterior translation with the arm in neutral rotation and a 6.3-mm increase in translation in internal rotation occurred.
Several other studies have examined the strain changes in the superior labrum and biceps anchor with different positions of the throwing motion. Pradhan et al found that a significant increase in strain in the anterior and posterior portions of the superior labrum only occurs when the arm is in maximum external rotation, as is the case in the late cocking phase.[15] Furthermore, the strain in the posterior portion of the superior labrum was significantly higher than that of the anterior portion.
Kuhn et al supported these findings with their study of failure patterns of the biceps superior labral complex.[16] They found that failure was significantly more likely in the late cocking position than in the early acceleration position. In the late cocking position, nine of 10 specimens demonstrated failure of the biceps superior labral complex. In contrast, of the 10 paired specimens that were tested in the early acceleration position, only two had failure of the biceps superior labral complex. The load to failure was found to be significantly less in the late cocking position than in the early acceleration position. Of the five type II SLAP lesions that developed, four were in the late cocking positions.
These studies emphasize the important role the biceps superior labral complex likely plays in anterior shoulder stability. An unstable SLAP lesion found in the course of a Bankart repair should be stabilized. The important role of the posterior portion of the superior labrum likely reflects the fact that the biceps tendon attachment is usually posterior-dominant, as demonstrated in a study by Vangsness et al.[10] In repairing SLAP lesions, particular attention should be given to ensuring the posterior aspect is well stabilized.
In considering the etiology of superior labral (labrum) lesions, it is useful to divide them into the the following two broad categories:
Clearly, engaging in throwing sports can predispose one to developing a SLAP lesion. The exact mechanism by which the lesion develops is somewhat controversial. In Andrews' original 1985 study, traction force placed on the superior labrum by the biceps tendon in the follow-through phase of the throwing motion was thought to be responsible for creating a SLAP lesion.[1] The hypothesis was that the eccentric contraction of the biceps necessary to decelerate the elbow resulted in the biceps tendon detaching portions of the glenoid labrum.
Subsequent studies, however, suggested that the forces generated during the late cocking phase are in fact the predominant factor. The peel-back mechanism described by Burkhart and Morgan[17] and the shear forces generated by a tight posteroinferior capsule are thought to be major contributing factors to developing type II SLAP lesions or variants thereof.
The presence of a peel-back sign can be demonstrated arthroscopically. The arm is placed into 70-90° of abduction and then progressively rotated externally. In this position, the biceps vector is now more posteriorly and vertically oriented. To accommodate this, the base of the biceps twists. A torsional load is transmitted to the superior labrum, and if the posterosuperior labrum and biceps anchor are incompetent, medial displacement of the superior labral biceps complex occurs. If more than 5 mm of the posterosuperior glenoid is uncovered or the biceps root at the level of the supraglenoid tubercle is uncovered, a posterior type II SLAP lesion is present.
As already noted, posterior capsule tightness is thought to play an important role in the development of SLAP lesions. Almost all high-demand throwers develop a posterior capsular contracture with limitation of internal rotation. This tight posteroinferior capsule is thought to result in obligatory superior translation of the humeral head when the arm is in abduction and external rotation and, as a result, exposes the superior labrum to large shear forces. This increased shear force is most pronounced at the same time the peel-back forces are at their maximum, increasing the likelihood of a SLAP lesion developing.
Superior labral (labrum) lesions are unusual. The reported prevalence in patients undergoing shoulder arthroscopy has ranged from 3.9% to 6%. In the largest series reported, SLAP lesions represented 6% of 2375 patients who underwent shoulder arthroscopy. The average age was noted to be 38 years, and 91% of the patients were male. The reported incidence of types I-IV is variable, with type II lesions being the most common. Type I lesions have been reported to account for 9.5-21% of all cases; type II, 41-55%; type III, 6-33%; and type IV, 3-15%.
Initial reports suggested good results with arthroscopic superior labral repairs with a high success both in nonthrowing and throwing athletes, as well as a high rate of overhead athletes returning to their preinjury level of activity.[18, 19] Morgan et al reported on their results in 102 patients,[8] with 83% having excellent results and 14% having good results. All pitchers returned to pitching, 84% of them at preinjury levels.
Pagnani et al reported that 12 of 13 overhead athletes were able to return to full preinjury level of activity after an arthroscopic superior labral tear.[20] Field and Savoie,[21] as well as Burkhart et al,[22] reported similar findings. In Field and Savoie's study, all of the athletes were able to return to sports activities without limitation.
However, it has become evident that overhead throwing athletes have poorer outcomes after superior labral repair compared with nonthrowers, with this being especially true if there is an associated rotator cuff tear, either partial or full thickness.[1, 3, 9, 17, 15] Furthermore within the overhead athlete group, baseball players have a lower rate of returning to preinjury level of activity.[12, 13]
Kim et al evaluated their results in 34 individuals who underwent arthroscopic suture anchor repair of an isolated SLAP (superior labrum, anterior and posterior) lesion tear.[23] Approximately 94% had a satisfactory result as determined by using the University of California Los Angeles (UCLA) shoulder score. Thirty-one (91%) of the patients regained their preinjury level of function. However, they did note poorer outcomes in overhead athletes compared with those not participating in overhead athletic activities.
In a prospective study, Brockmeier et al reviewed their outcomes after arthroscopic repair of a type II SLAP tear in 47 patients and reported that 87% had a good or excellent result.[24] However, only 74% of the patients were able to resume their preinjury level of athletics. They also found patients with a discrete traumatic event had a greater likelihood of resuming preinjury level of activity. In a subgroup of 12 athletes who had discreet traumatic event, 11 (92%) were able to resume preinjury level of activity.
Neuman et al retrospectively reviewed their results of type II superior labral repair in 30 overhead athletes.[25] Overall, 93% had good-to-excellent results and 84% returned to preinjury level of play. However, with subgroup analysis, baseball players only had an 80% return to preinjury level of play compared with 94% for other overhead athletes.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved