

Although the concept of anterior shoulder instability has been described in the medical literature since the time of Hippocrates, the recognition of posterior instability of the glenohumeral joint has been much more recent. Sir Astley Cooper is credited with the first medical description of a posterior shoulder dislocation, in 1822.[1] He later described the "dislocation of the os humeri upon the dorsum scapula" as "an accident which cannot be mistaken."[2]
Since Cooper's time, numerous articles have gradually raised physician awareness of this condition. In 1952, Harrison McLaughlin defined posterior dislocation as a "diagnostic trap," and others have used equally foreboding descriptions.[3] Even today, the diagnosis of posterior shoulder dislocation continues to be missed or diagnosed late, after the patient has undergone unsuccessful and often painful therapy for adhesive capsulitis.
Despite the supposed diagnostic difficulty spoken of even today for posterior shoulder dislocations, orthopedic history would indicate otherwise. In 1855 (40 years before the development of radiographs), the French surgeon Joseph Malgaigne published a paper that detailed three of his own patients (and 34 from the literature) that had been diagnosed purely on the basis of physical examination.[4, 5] McLaughlin also stated that "the clinical diagnosis is clear-cut and unmistakable, but only when the posterior subluxation is suspected."[6] It also might be said that knowledge of a particular diagnosis statistically increases the likelihood of the clinician making that diagnosis.
In 1949, Wilson and McKeever reported on 11 patients with posterior shoulder dislocations.[7, 8] Seven of the injuries occurred as a result of trauma, three were due to "epileptic convulsions," and one was due to electrocution. Key clinical findings regarding posterior shoulder dislocations were highlighted by these authors. These included the following:
For some acute dislocations, Wilson and McKeever recommended that a Velpeau bandage be applied with the patient's shoulder fully internally rotated and with the forearm lying across the small of the patient's back (a position now commonly used at the beginning of the liftoff test for subscapularis function).
Posterior glenohumeral instability is much less common than anterior instability. However, the condition has been recognized with increased frequency; this may be due to improved awareness of the entity, an increasingly athletic population, or both. In early reports of posterior instability, the terminology of instability was confusing, and chronic locked posterior dislocations were often combined with recurrent instabilities.
Each of these conditions has provided physicians with a dilemma not only in diagnosis but also in formulating an ideal treatment plan. The symptoms of posterior instability may mimic those of other disorders, and because complete dislocation does not always occur, the diagnosis cannot be confirmed readily with radiographs.
Advances in arthroscopic techniques hold interesting potential for the management of posterior instability. Long-term studies, however, are not yet available. Another area of interest has been thermal capsulorrhaphy for instability of the shoulder.[9, 10] Many authors have described techniques for arthroscopic capsular shrinkage procedures for shoulder instability; however, no outcome studies are available yet for the treatment of isolated posterior instability. This approach may hold promise as an isolated procedure or in combination with other arthroscopic techniques. Short-term results have been encouraging, but longer-term follow-up and published, peer-reviewed studies are required.
The purpose of this article is to review current knowledge about the diagnosis, classification, and treatment of posterior glenohumeral instability.[11]
NextThe anatomy relevant to surgical treatment for posterior shoulder instability is related to the posterior approach to the glenohumeral joint. Two general posterior approaches to the glenohumeral joint have been described.
In 1944, Rowe and Yee presented a posterior approach to the shoulder using a linear incision over the entire length of the scapular spine, extending to the posterior corner of the acromion.[12] The origin of the deltoid on the scapular spine is identified and detached from lateral to medial. The interval between the infraspinatus and the teres minor is defined and retracted to expose the posterior aspect of the joint capsule.
In 1993, Wirth et al described the posterior deltoid-splitting approach to the shoulder.[13] Their technique allows preservation of the deltoid origin from the scapular spine and posterior acromion. (In more traditional posterior approaches to the shoulder joint, part or all of the origin of the deltoid is detached.) This approach therefore maintains the strength and function of the posterior deltoid.
Several structures are at risk during the posterior dissection of the shoulder. The axillary nerve runs through the quadrilateral space beneath the teres minor and can be injured if the interval between the infraspinatus and the teres minor is not critically defined. The suprascapular nerve passes around the base of the spine of the scapula as it runs from the supraspinatus fossa to the infraspinatus fossa. The infraspinatus must not be retracted forcefully too far medially during the approach, because a neurapraxia may result from stretching the nerve around the unyielding lateral edge of the scapular spine.
The posterior circumflex humeral artery runs with the axillary nerve in the quadrilateral space beneath the inferior border of the teres minor muscle. Damage to this artery leads to hemorrhaging that is difficult to control; injury to the artery can be avoided by staying in the correct intermuscular plane.
Posterior glenohumeral instability can be associated with several anatomic conditions. Bony anatomic deformities that have been implicated include increased humeral retroversion, glenoid retroversion, and glenoid hypoplasia.[7, 8, 14, 15] When the bony anatomy is normal, the pathoanatomy often is attributed to the following:
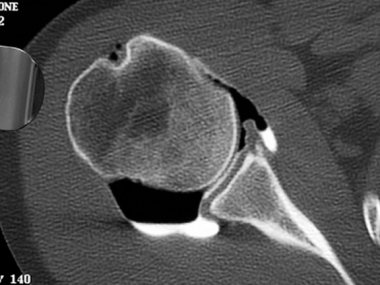 Computed tomography (CT) arthrogram of a shoulder with atraumatic posterior instability demonstrates a patulous posterior capsule consistent with excessive capsular laxity.
Computed tomography (CT) arthrogram of a shoulder with atraumatic posterior instability demonstrates a patulous posterior capsule consistent with excessive capsular laxity.
Many authors have emphasized that posterior stability is heavily dependent on the integrity of the inferior glenohumeral ligament.[25, 26, 27, 28]
Alteration of the stabilizing forces of the glenohumeral joint has been implicated in contributing to the pathophysiology of posterior instability. Posterior instability usually occurs in midrange shoulder motion when the stabilizing ligaments of the humeral head are not under tension. Therefore, disruption of the capsuloligamentous structures cannot be solely responsible for instability. Three mechanisms that have been identified as the primary stabilizing forces of the glenohumeral articulation during the midrange motion are as follows[29, 30] :
An alteration of one or more of these stabilizing forces, therefore, contributes to posterior instability.
The contribution of the rotator interval also has been recognized as an important static restraint in preventing posterior and inferior instability. In their cadaveric study, Harryman et al reported that imbrication of the rotator interval assists in preventing posterior and inferior instability.[31] Selective cutting studies of the glenohumeral joint also have determined the importance of the anterior ligamentous structures on posterior instability.[32]
Labral injury has been described in association with posterior instability (see the image below). Pathologic lesions have been identified, such as the posterior labral tear; posterior capsular stripping or laxity; fracture, erosion, sclerosis and ectopic ossification of the posterior glenoid fossa; and reverse Hill-Sachs lesions.[33] Labral lesions have also been described in the impact athlete in whom the posterior glenohumeral compressive force is increased.[34] This causes a greater resultant shear force imparted to the posterior labrum and articular surfaces with forced translation.
 Arthroscopic examination of a patient with recurrent posterior instability reveals significant fraying and tearing of the posterior labrum.
Arthroscopic examination of a patient with recurrent posterior instability reveals significant fraying and tearing of the posterior labrum.
An isolated pathologic lesion responsible for posterior instability is rare. Posterior instability is typically multifactorial in nature, and accurately identifying all the causative agents preoperatively is difficult. The operating surgeon must be aware of all potential pathophysiologic clues so that when identified during the operative procedure, these causes can be corrected.
An absolute definition of shoulder instability is difficult to formulate and has been the center of a vast amount of research. Whereas isolated traumatic dislocations can be described by their relationship to the bony landmarks of the shoulder, instability without formal dislocation may be much more difficult to ascertain. One must differentiate between shoulder laxity, which is a physiologic variant of normal, and shoulder instability, which is a symptomatic, pathologic process.
Posterior glenohumeral dislocations typically lie behind the glenoid and beneath the acromion (subacromial). In rare instances, the humeral head may be positioned behind and under the glenoid (subglenoid) or medial to the acromion and beneath the scapular spine (subspinous).[35]
Hawkins and McCormack described three categories of posterior glenohumeral instability, as follows[36] :
In the third category, the voluntary group was subdivided into the habitual (willful) subluxation secondary to personality disorder and subluxation caused by voluntary muscle control. The involuntary group was subdivided into positional (not willful but demonstrated by the patient) and nonpositional (not demonstrable by the patient).
Other classification systems also have been described for posterior glenohumeral instability. Dimon classified posterior dislocations according to the mechanism of injury, as follows[37] :
Instability or subluxation of the glenohumeral joint has been simply classified according to whether it results from a traumatic or a nontraumatic injury. It can be subdivided into voluntary and involuntary cases.[35] The direction of instability also has been used to classify the pathology.[38] The direction of instability can be unidirectional (posterior only), bidirectional (posterior and inferior), or multidirectional (posterior, inferior, and anterior) and is important to determine in planning the surgical approach.
Posterior shoulder instability is also a well-recognized consequence of neonatal brachial plexus injury, such as Erb palsy. Such dislocations have been reported in children as young as 6 months.[39] Waters et al, from Boston Children's Hospital, used computed tomography (CT) or magnetic resonance imaging (MRI) to prospectively study 42 patients with birth palsy.[40] They found a 62% rate of posterior shoulder subluxation. Persistent internal rotation contracture is thought to be the primary culprit responsible for significant glenoid dysplasia (and resultant posterior instability) that is typically quite advanced by age 2 years.[41]
Posterior instability is thought to be secondary to three types of etiologic processes, as follows[20, 42, 43] :
Major injury of the glenohumeral joint can occur directly or indirectly to the shoulder.
Direct trauma to the anterior shoulder or axial loading of a flexed, adducted, internally rotated arm may cause a posterior dislocation. Indirectly, posterior dislocations can occur secondary to violent muscle contractions associated with seizures or electrical shock. In this condition, the strong internal rotation forces of the latissimus dorsi, the pectoralis major, and the subscapularis overpower the relatively weaker external rotator muscles.[25]
Pure, isolated, unidirectional posterior subluxation of the glenohumeral joint is rare.[38, 16] Most cases have either an inferior component (bidirectional) or inferior and anterior components (multidirectional), secondary to generalized ligamentous laxity or to repetitive microtrauma causing either stretching of the static restraints or weakness of the dynamic restraints.
Recurrent posterior instability of the glenohumeral joint is less common than anterior instability, representing fewer than 5% of shoulder dislocations in most series.[20] Early in the published experience, McLaughlin reported 22 posterior dislocations or subluxations in 581 shoulder dislocations, an incidence of 4%.[3] In subsequent publications, the incidence was reported to be 2-12% of all cases of shoulder instability.[44]
Historically, surgical repairs for posterior instability have had mixed results, with failure rates as high as 50% reported in the literature. Overall, surgical intervention is associated with a 50-95% success rate.[45, 46, 47, 48] Because of differences regarding classification and terminology, most studies have combined groups of patients with trauma, multidirectional laxity, unidirectional or multidirectional instability, voluntary subluxation, and intentional or positional instability. Consequently, the results of treatment are often not reported for one well-defined variant of the condition.
The rates of recurrence after a posteroinferior capsular shift procedure for posterior instability are higher than the rates of repair for anterior instability. Nonetheless, most shoulders improve from the procedure, and the patients are satisfied. The rate of recurrence after a posteroinferior capsular shift performed as a posterior revision operation is prohibitive when the infraspinatus or the deltoid has been damaged.[22, 49] The best procedure for posterior instability, however, is currently unknown; the technique, therefore, must be individualized to the specific needs of the patient.
Within the context of a 2- to 5-year follow-up, reduction of posterior shoulder dislocation in younger children appears to be associated with improved shoulder motion and function. Hoffer has recommended that in such situations, reduction of the shoulder joint should be accompanied by release of the pectoralis major and transfer of the latissimus dorsi and the teres major.[50, 51] In older children (Hoffer suggests age 7 years as a possible threshold), rotational osteotomy is an option.
Kirkos and Papadopoulos reported on 22 of their rotational osteotomy patients (age range, 4-17 years), four of whom demonstrated posterior shoulder subluxation. Improved function in activities of daily living was documented, as were average increases in abduction and rotation of about 25°.[52] The images below illustrate the anteroposterior (AP), scapular-Y, and axillary radiographs of the right shoulder of a 7-year-old girl with severe upper brachial plexus palsy. Note the marked glenohumeral dysplasia and frank posterior shoulder dislocation. The child's severe loss of shoulder motion prevented her from performing many activities, including combing her own hair.
 Anteroposterior radiograph of 7-year-old girl with brachial plexus palsy.
Anteroposterior radiograph of 7-year-old girl with brachial plexus palsy.
 Scapular-Y view.
Scapular-Y view.
 Axillary view.
Axillary view.
After rotational osteotomy her function (including the ability to comb her hair) was significantly improved (see the images below).
 Postoperative anteroposterior radiograph showing healed osteotomy site.
Postoperative anteroposterior radiograph showing healed osteotomy site.
 Postoperative lateral radiograph.
Postoperative lateral radiograph.
In a systematic review and meta-analysis of the available literature on clinical outcomes for posterior shoulder instability, DeLong et al reached the following conclusions[53] :
Copyright © www.orthopaedics.win Bone Health All Rights Reserved