

Ruptures of the quadriceps tendon occur relatively infrequently and usually occur in patients older than 40 years. A strong association exists with numerous systemic diseases and prior degenerative changes in the knee extensor mechanism. Ruptures most often occur unilaterally. Bilateral ruptures are highly correlated with systemic disease but have been reported in healthy patients who do not have predisposing factors.[1, 2, 3, 4, 5, 6, 7, 8]
Patellar tendon ruptures are less common than are quadriceps ruptures and tend to occur in patients younger than 40 years. In rare cases, partial ruptures of the quadriceps tendon are seen in young athletes with end-stage jumper's knee.[9, 10, 11, 12] Jumper's knee usually involves the patellar tendon, although in 25% of cases, the quadriceps is involved. To obtain the best results, the early diagnosis and repair of complete quadriceps ruptures are essential.[13] If intervention is delayed, repair is more difficult and results may be compromised.
An image depicting tendon rupture can be seen below.
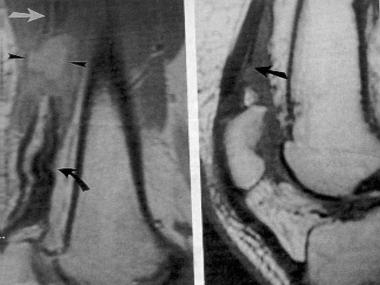 Magnetic resonance imaging (MRI) scans of complete and incomplete quadriceps tendon ruptures. Reproduced with permission from Zeiss J, Saddemi SR, Ebraheim NA. MR imaging of the quadriceps tendon: normal layered configuration and its importance in cases of tendon rupture. AJR Am J Roentgenol. Nov 1992;159(5):1031-4.
Next
Magnetic resonance imaging (MRI) scans of complete and incomplete quadriceps tendon ruptures. Reproduced with permission from Zeiss J, Saddemi SR, Ebraheim NA. MR imaging of the quadriceps tendon: normal layered configuration and its importance in cases of tendon rupture. AJR Am J Roentgenol. Nov 1992;159(5):1031-4.
Next
Galen first reported the extensor mechanism injury around 130-201 CE. He described a young man injured during a wrestling match. Several other authors wrote on the subject during the 1700s and 1800s, including Ruysch, Louis Petit, Dupuytren, and Samuel. Treatment was nonoperative. In 1878, Lister was the first to report on surgical repair. In 1887, McBurney reported on the first surgical repair in the United States. The injury was a direct blow to the knee, and the tendon was repaired using catgut and silver wire. After several other reports on surgical repair of extensor mechanism injuries were published in the early 1900s, operative management became standard.
In 1949, Steiner and Palmer reported the first case of bilateral, simultaneous ruptures of the quadriceps tendons. Since then, several large series of patients undergoing quadriceps tendon repair have been published. These include works by Scuderi in 1958, Ramsey and Muller in 1970,[14] Siwek and Rao in 1981,[15] Larsen and Lund in 1986,[16] Rasul and Fischer in 1993,[17] Rougraff and colleagues in 1996,[18] and Konrath and co-authors in 1998.[19] Many case reports of bilateral quadriceps ruptures have been published in the last few decades.[2, 3, 4, 5, 6, 7]
Complete quadriceps tendon rupture is a disabling injury, and operative repair is required to obtain an optimal result.
Unilateral ruptures are relatively rare when all types of knee injuries are considered; bilateral ruptures are even less common. However, quadriceps tendon ruptures are more common than are patellar tendon ruptures, although quadriceps tendon ruptures are more likely to be misdiagnosed.[20]
As mentioned previously, quadriceps tendon rupture usually occurs in patients with predisposing factors who are older than 40 years, but these ruptures may be seen in nearly any age group. Siwek and Rao reviewed 69 cases reported in the literature from 1880-1978 and found that 88% of the ruptures were in patients aged 40 years or older.[15] To the authors' knowledge, the youngest patient was a 13-year-old who had been immobilized in a long-leg cast prior to injury.
In contrast, partial ruptures occur in young athletes.[9, 10, 11, 12] Raatikainen and colleagues reported an average age of 28 years in a series of patients with partial tears.[21] Partial and complete tears occur predominantly in males.
Quadriceps tendon rupture usually occurs during a rapid, eccentric contraction of the quadriceps muscle, with the foot planted and the knee partially flexed. This injury commonly occurs during falls. Other mechanisms of injury include direct blows, lacerations, and iatrogenic causes.[22, 23, 24, 25, 26, 27, 28, 29, 30]
McMaster showed that normal tendons in rabbits do not rupture under stress. Instead, linear stress causes disruption at the musculotendinous junction, the muscle belly, or the tendinous insertion into bone. Harkness demonstrated that approximately 30 kg/mm2 of longitudinal stress may be applied to normal quadriceps tendons prior to failure. Additionally, many ruptures occur after relatively trivial trauma. Therefore, tendon rupture usually occurs through a pathologic area of the tendon.
Many conditions have been reported to contribute to degeneration of the quadriceps tendon, including the following:
Repetitive motion has been implicated as the cause of jumper's knee.[33, 34]
Rare iatrogenic cases have been reported. Examples include rupture after total knee arthroplasty (TKA), lateral retinacular release, meniscectomy, and anterior cruciate ligament (ACL) reconstruction with central-third patellar tendon graft. In addition, steroid injections are believed to weaken tendons. Quadriceps tendon ruptures have also reportedly occurred with knee and patellar dislocations.
Quadriceps tendon rupture usually occurs distally 0-2 cm from the superior pole of the patella, through pathologic tissue. Various systemic conditions may cause damage to the tendon vascular supply or may disrupt the tendon structure. Diabetes can cause arteriosclerotic changes in tendon vessels. Fibrinoid necrosis of tendons is seen with chronic synovitis. Hyperparathyroidism causes dystrophic calcifications and subperiosteal bone resorption at the tendon insertion. Obesity causes fatty degenerative changes in tendons and increases the forces on the tendon. Fatty degeneration, fibrinoid degeneration, and decreased collagen are seen with normal aging.
Kannus and Jozsa examined histopathologic changes in 891 ruptured tendons; about 97% of the pathologic changes were degenerative.[35] The degenerative changes included hypoxic degenerative tendinopathy, mucoid degeneration, tendolipomatosis, and calcifying tendinopathy. In the 82 quadriceps tendons, tendolipomatosis was the most common type of degeneration, seen in almost half of the tendons (see image below).
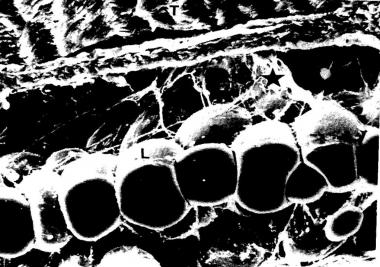 Tendolipomatosis. Reprinted with permission from Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am. Dec 1991;73(10):1507-25.
Tendolipomatosis. Reprinted with permission from Kannus P, Józsa L. Histopathological changes preceding spontaneous rupture of a tendon. A controlled study of 891 patients. J Bone Joint Surg Am. Dec 1991;73(10):1507-25.
No signs of inflammatory cells were noted in any of the specimens. In 62% of the ruptured tendons, pathologic changes of the tendon blood supply were seen, including vessel narrowing and thrombosis. These findings led the investigators to suggest that nutrition and decreased blood flow, resulting in local hypoxia and impaired metabolic activity, are key factors in tendon degeneration.[36]
Patients typically present with acute knee pain, swelling, and functional loss following a stumble, fall, or giving way of the knee. There may be no history of prior knee pain. However, younger patients with jumper's knee usually have a history of chronic, activity-related pain above the patella that is exacerbated by jumping or kneeling. Specifically ask patients about any history of systemic disease, steroid use, infection, tumors, or prior surgeries. There may be a history of an audible pop at the time of injury.
Begin the physical examination by noting any obesity. Patients with recent ruptures have difficulty ambulating. Usually, obvious suprapatellar swelling, ecchymosis, and tenderness are present. Carefully evaluate lacerations. There may be a palpable defect in the suprapatellar area and a low-lying patella, but swelling initially may obscure this finding.
Testing for full, active extension against gravity is the most important aspect of the examination. This may make the defect more apparent. Extension lags of varying degrees are seen, depending on the amount of retinacular damage. In incomplete ruptures, the patient may be able to fully extend the knee from the supine position but not from the flexed position. If only tendinitis is present, no extension lag should be noted with any test position. Examine the contralateral knee to rule out bilateral rupture.
If the patient is not seen in the acute phase, diagnosing the rupture becomes more difficult, and it can be easily missed. Ramsey and Muller reported misdiagnosis in 7 of 17 ruptures.[14] Patients with quadriceps tears, especially elderly patients, have been identified as having had and having been treated for strokes, radiculopathy, and myelopathy. Many patients are thought to have only simple knee sprains during their examination in the emergency room and are not given appropriate, immediate follow-up.
Pain and swelling decrease over time, and quadriceps function can improve. Patients may be able to ambulate but will do so with a gait demonstrating knee stiffness and elevation of the hip to accommodate the swing-through phase. In addition, patients may have frequent buckling of the knee and difficulty with stair climbing.
Results of neurologic examination are normal except for decreased quadriceps motor function and an absent patellar reflex. Again, full, active knee extension against gravity is the key component of the physical examination.
Early operative repair is indicated for all acute, complete quadriceps tendon ruptures, provided that the patient is a suitable surgical candidate. Surgery is also indicated for most chronic, complete quadriceps ruptures. Although repair/reconstruction is technically more difficult and results are inferior to those of early repair, successful results have been reported with surgery performed even as late as a year following injury. Partial tears may be treated nonoperatively unless they are refractory to a long course of conservative management.
The quadriceps muscle is composed of four muscle groups, as follows:
The quadriceps tendon is formed by the convergence of all four muscles just proximal to the superior patella. The tendon is multilayered. The rectus femoris becomes tendinous 3-5 cm proximal to the patella and is the most superficial layer inserting on to the patella. Some of its fibers continue over the anterior patellar surface and contribute distally to the patellar tendon. The middle layer is composed of the vastus lateralis and vastus medialis.
The vastus medialis, which is composed of the vastus medialis obliquus and the vastus medialis longus, becomes tendinous only a few millimeters from its insertion into the patella. The vastus lateralis becomes tendinous about 3 cm proximal to its insertion into the patella. The deep layer is composed of the vastus intermedius. The tendon has an average thickness of 8 mm and an average width of 35 mm.
Peterson et al found that the blood supply to the quadriceps tendon arises from the descending branches of the lateral circumflex femoral artery, branches of the descending geniculate artery, and branches of the medial and lateral superior geniculate arteries.[37] The superficial layers are well vascularized. In the deep layer, however, there is an oval, avascular area that is 30 × 15 mm in size; it probably plays a significant role in tendon degeneration.
No contraindications for acute repair of quadriceps tendon ruptures exist provided that the patient is an adequate surgical candidate. For delayed repair/reconstruction, no contraindications for surgery appear to exist up to 1 year following injury. The authors are unaware of any literature on operative management performed later than 1 year following rupture.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved