

Plica syndrome of the knee is a constellation of signs and symptoms that occur secondary to injury or overuse. Plica is a Latin word meaning "fold." This term is simply a descriptive one; there is no empiric evidence that true folding of the synovial lining ever occurs.
Synovial plicae are normal structures found in many knees. Under normal circumstances, these plicae are not associated with any painful conditions. However, with the right combination of events they can become quite painful.[1] These events almost certainly include a somewhat exuberant plical shelf at baseline combined with an inciting event (either discrete macrotrauma or repeated microtrauma). Once an inflammatory process is established, the normal plical tissue may hypertrophy into a truly pathologic structure (see the image below).[2]
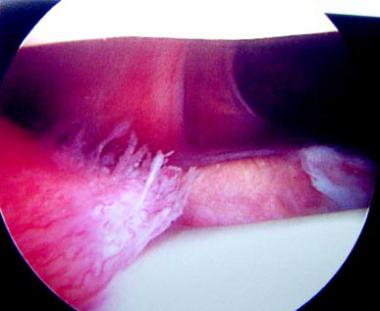 Plica syndrome. Typical appearance of a large beefy medial parapatellar plica.
Plica syndrome. Typical appearance of a large beefy medial parapatellar plica.
Both the normal and the pathologic aspects of various synovial plicae readily became apparent to orthopedic surgeons with the advent of arthroscopy. Arthroscopy is a Japanese innovation that changed the face of orthopedics forever. Kenji Takagi (1888-1963) and Masaki Watanabe and others in Japan drove its early development, and early adopters in North America, such as Robert Jackson and Lanny Johnson, helped popularize this technology.[3, 4]
Future treatment of plica syndrome may be supplemented further by improved brace designs and pharmacologic treatments. Earlier recognition of patients with the syndrome might facilitate syndrome resolution by such means, in contrast to patients who experience years of symptoms.
This article provides an overview of the pertinent anatomy and of diagnosis and treatment of plica syndrome of the knee.[5, 6]
NextDuring embryonic development, the knee is divided initially by synovial membranes into three separate compartments. By the third or fourth month of fetal life, the membranes are resorbed, and the knee becomes a single chamber. If the membranes resorb incompletely, various degrees of septation may persist. These embryonic remnants are known as synovial plicae. Four types of synovial plicae of the knee have been described in the literature.[7, 8]
The suprapatellar plica (plica synovialis suprapatellaris) divides the suprapatellar pouch from the remainder of the knee. Rarely, it may initiate a suprapatellar bursitis or perhaps chondromalacia, and symptoms secondary to these conditions may be present.[9] Anatomically, this plica can be complete or in the form of a porta, which only partially separates the compartments. It courses from the anterior femoral metaphysis or the posterior quadriceps tendon to the medial wall of the joint. It usually begins proximal to the superior pole of the patella but may begin anywhere.
The mediopatellar plica (referred to by some as the Aoki ledge or Iino band) is the most frequently cited cause of plica syndrome. It lies on the medial wall of the joint, originating suprapatellar, and courses obliquely down to insert on the infrapatellar (ie, Hoffa) fat pad. This plica, sometimes known as a shelf, lies in the coronal plane.[10, 11, 12]
The rare and poorly documented lateral synovial plica is a wider and thicker band than the medial plica. It is located along the lateral parapatellar synovium, inserting on the lateral patellar facet and extending distally toward the infrapatellar region. It has been argued that the lateral plica, rather than being a vestigial septum, is derived from the parapatellar adipose synovial fringe.
The plica that is the least symptomatic of all, the infrapatellar plica (ligamentum mucosum) is, ironically, the one most commonly encountered. Some authors even claim that the infrapatellar plica is never responsible for plica syndrome. This bell-shaped remnant originates in the intercondylar notch, widens as it sweeps through the anterior joint space, and attaches to the infrapatellar fat pad. This plica's ability to obscure portal entry sites or interfere with visualization during arthroscopy is touted as its only significance. Kim et al classified ligamentum mucosum (ie, infrapatellar plica) into the following five groups[13] :
In a clinical study of 400 knees in more than 350 patients, Kim and Choe found suprapatellar plicae in 87%, mediopatellar plicae in 72%, infrapatellar plicae in 86%, and lateral plicae in 1.3%.[14]
Not all synovial plicae are symptomatic. For those that are, the cause may not always be apparent.
Inflammation leads to edema, thickening, and decreased elasticity of the plica. The plica may develop irregular edges and may snap over the femoral condyle, leading to a secondary synovitis and chondromalacia. Loose areolar fatty tissue appears to become gristlelike, and when plicae are soft, wavy, and vascular with synovial-covered edges, they are not pathologic. Numerous studies describe pathologic plicae as thick, fibrotic, white, and inelastic. Histologically, fibrosis, hyalinization, and calcification are present.[15]
The etiology of symptomatic plica is unclear. Potential causes of inflammation include repetitive stress, a single blunt trauma, loose bodies, osteochondritis dissecans, meniscal tears, or other aggravating knee pathology. The most common symptomatic plica is medial plica; occasionally, suprapatellar plica may also be symptomatic.[16, 17, 18, 19, 20]
A popular theory for the initiation of inflammation is that the plica is converted to a bowstring, which causes it to contact the medial femoral condyle. During flexion of the knee, the plica causes an abrasion to the condyle, resulting in symptoms. Others contend that a plica need not contact the femoral condyle to cause symptoms.
One study found that the onset of symptoms was usually delayed until adolescence. Possible explanations include a decrease in tissue elasticity with age, and a biomechanical change resulting from a growth spurt.
The precise incidence of plica syndrome is a source of ongoing controversy. The incidence of symptomatic or pathologic plica versus asymptomatic plica is even more debatable. Some authors contend that distribution is regional. Distribution differences based on race or ethnicity may exist.
The incidence of suprapatellar plica has been reported to be as low as 11%; however, one study reported a rate of 89% on autopsy.
Medial plica has a reported incidence of 18-60%. The incidence of medial plica in anatomic studies is similar to that in arthroscopic studies. The most commonly cited incidence figure in the literature is approximately 20-25%. Nakayama investigated the incidence of medial plicae in 3889 knee joints in the Japanese population and classified the plicae into four types according to Sakakibara’s classification, as follows[21] :
The incidence of medial plicae was 79.9%; the incidence of Sakakibara types A, B, C, and D medial plicae was 35.2%, 22.4%, 12.3%, and 10%, respectively.[21]
Little literature exists on lateral plica. Most of this literature is Japanese, and few cases have been reported in English.[22] Incidence of this kind of plica is less than 1%.
Dupont et al found some type of inferior plica in 65% of their 200 dissected cadaveric knees. They stated that it was the most frequently found plica. In their review of the literature, infrapatellar plica was most common in some studies but not in others.[7]
The outcome of surgical treatment for well-selected patients with plica syndrome is very good.[23, 24, 25] A clinical trial conducted by Johnson et al in England demonstrated a success rate of more than 80%.[26] In this same study, nearly 50% of patients in the control group experienced continued symptoms severe enough that they later returned for definitive arthroscopic resection of their plicae.
In a predominantly adult population (average age, 25 years; range, 11-56 years), Kasim and Fulkerson reported 88% moderate-to-substantial improvement at an average of more than 4 years after resection of localized segments of painful retinacula (ie, plicae) about the knee.[27]
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved