

Fractures of the acetabulum occur primarily in young adults as a result of high-velocity trauma (eg, vehicular accidents or falls from heights). These fractures are often associated with other life-threatening injuries.
Displacement of the fracture fragments leads to articular incongruity of the hip joint that results in abnormal pressure distribution on the articular cartilage surface. This can lead to rapid breakdown of the cartilage surface, resulting in disabling arthritis of the hip joint.[1] Anatomic reduction and stable fixation of the fracture, such that the femoral head is concentrically reduced under an adequate portion of the weightbearing dome of the acetabulum, is the treatment goal in these difficult fractures.
Fractures of the acetabulum were treated nonoperatively until the middle of the 20th century. The Judet brothers and, subsequently, Emile Letournel studied acetabular fractures extensively and were responsible for popularizing the surgical management of these challenging injuries.[2, 3, 4] Pioneering work, such as the development of the ilioinguinal approach by Letournel, led to acetabular surgery becoming the accepted standard of care for virtually all displaced fractures of the acetabulum.[5]
With advances in imaging technologies, performing acetabular fracture surgery through smaller incisions is now possible. In the future, computer-assisted surgery may contribute to the operative management of these injuries, as well.
NextThe acetabulum is formed by a portion of the innominate bone. It lies at the point where the ilium, ischium, and pubis are joined by the triradiate cartilage, which later fuses to form the innominate bone. The acetabulum is enclosed by the anterior and the posterior columns like the two limbs of an inverted Y (see the images below).
 Columns of the acetabulum, anteroposterior view. The white area is the anterior column, the red area is the posterior column, and the purple area is the tie beam (inferior pubic ramus).
Columns of the acetabulum, anteroposterior view. The white area is the anterior column, the red area is the posterior column, and the purple area is the tie beam (inferior pubic ramus).
 Columns of the acetabulum, iliac view.
Columns of the acetabulum, iliac view.
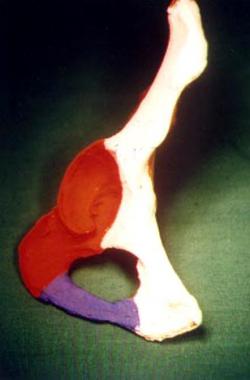 Columns of the acetabulum, obturator view.
Columns of the acetabulum, obturator view.
The anterior column comprises the anterior border of the iliac wing, the entire pelvic brim, the anterior wall of the acetabulum, and the superior pubic ramus. The posterior column makes up the ischial portion of the bone, including the greater and lesser sciatic notch, the posterior wall of the acetabulum, the majority of the quadrilateral surface, and the ischial tuberosity. The roof of the acetabulum is the thick, weightbearing portion and forms a separate fragment in bicolumnar fractures. The thin quadrilateral plate forms the medial wall or the floor of the acetabulum.
The innominate bone is irregular in shape and has differing thickness in cross-section in different areas. The posterior column and sciatic buttress provide the best purchase for screws. The areas suitable for implant placement are shown in the images below.[6]
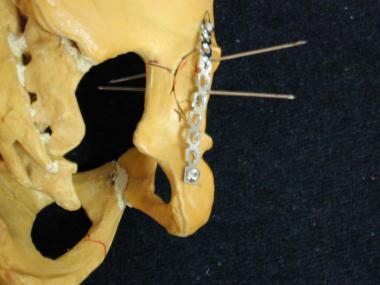 Fixation of posterior wall fracture: Bone model showing the direction of screws and application of neutralization/buttress plate.
Fixation of posterior wall fracture: Bone model showing the direction of screws and application of neutralization/buttress plate.
 Posterior wall fracture: Postoperative anteroposterior (AP) view.
Posterior wall fracture: Postoperative anteroposterior (AP) view.
 Posterior lip fracture: Postoperative iliac view.
Posterior lip fracture: Postoperative iliac view.
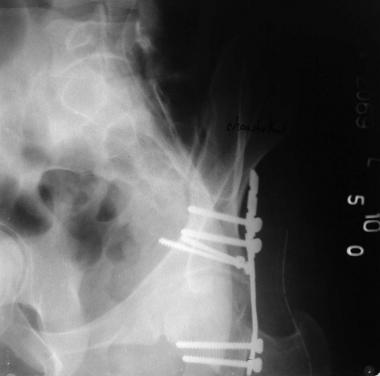 Posterior wall fracture: Postoperative obturator view.
Posterior wall fracture: Postoperative obturator view.
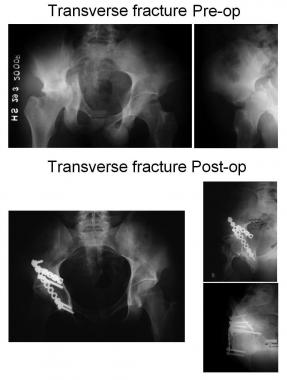 Transverse fracture.
Transverse fracture.
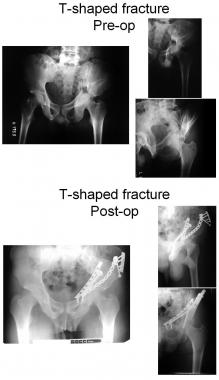 T-shaped fracture (note the use of the anterior-to-posterior lag screw to hold the posterior column).
T-shaped fracture (note the use of the anterior-to-posterior lag screw to hold the posterior column).
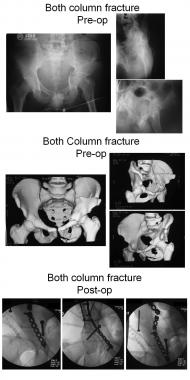 Both-column fracture.
Both-column fracture.
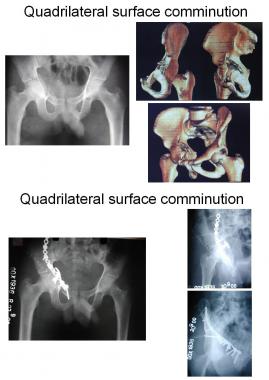 Quadrilateral surface comminution: Use of a T-plate.
Quadrilateral surface comminution: Use of a T-plate.
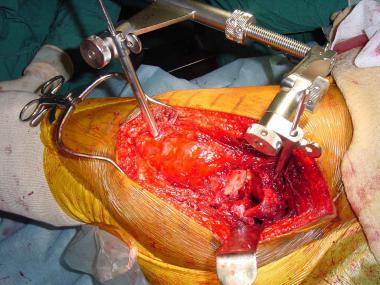 Use of femoral distractor during surgery.
Use of femoral distractor during surgery.
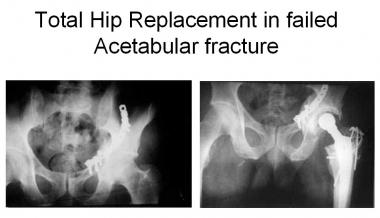 Total hip replacement in posttraumatic arthritis after an acetabular fracture.
Total hip replacement in posttraumatic arthritis after an acetabular fracture.
 Intra-articular screw as seen on the axial cut of the CT scan.
Intra-articular screw as seen on the axial cut of the CT scan.
An intimate knowledge of the nerves and vessels in the area is essential to prevent iatrogenic complications at the time of surgery. Details of the relevant anatomy are elaborated further in the discussion on surgical approaches (see Treatment).
Fractures of the acetabulum occur as a result of the force exerted through the head of the femur to the acetabulum. The femoral head acts like a hammer and is the last link in the chain of forces transmitted from the greater trochanter, knee, or foot to the acetabulum. The position of the femur at the time of impact and the direction of the force determine the type and displacement of the fracture.
Although it is difficult to pinpoint the exact relation between the point of impact and the mechanism of injury in acetabulum fractures, certain relations are well recognized. These can help in understanding the forces involved in creating the fracture, the direction of displacement, and the fracture patterns involved.
Force applied to greater trochanter in axis of femoral head
The point of impact of the femoral head is decided by the degrees of adduction and abduction and rotation of the femur.
With the hip in neutral adduction-abduction, external rotation of the hip predisposes to anterior column injury, and internal rotation predisposes to posterior column injury. Rotations and associated fractures are as follows:
With the hip in neutral rotation, the greater the degree of adduction of the femur, the higher the level of the fracture (greater involvement of the roof). The greater the degree of abduction, the lower (more inferior) is the fracture line. Positions of the femur and associated fractures are as follows:
Force applied to flexed knee in axis of femoral shaft
Acetabulum fracture morphology depends on the degrees of flexion or extension and adduction or abduction. The degree of hip rotation generally does not contribute significantly to the fracture pattern.
With the hip flexed to 90°, positions of the femur and associated fractures are as follows:
With different degrees of hip flexion, positions of the femur and associated fractures are as follows:
Force applied to foot with knee extended
Positions of the femur with associated acetabulum fractures are as follows:
Force applied to lumbosacral region
A force applied to the lumbosacral region is a rare cause of acetabular fractures.
In actuality, however, it is very difficult to pinpoint the exact site of impact and the mechanism of injury. These mechanisms are important, in that they help in understanding the acting forces, direction of displacement, and the fracture patterns involved.
Various classifications of acetabular fractures have been propounded, but the easiest classification is that of Judet and Letournel, who classified acetabular fractures according to the fracture morphology as elementary fracture patterns.[2, 3] These have only one fracture line and include the following:
Posterior-wall fractures (see the images below) typically involve the rim of the acetabulum, a portion of the retroacetabular surface, and a variable segment of the articular cartilage. The articular cartilage may also be impacted. Impacted articular cartilage should be diagnosed preoperatively on computed tomography (CT); these impacted fragments require elevation at the time of surgery.
 Posterior wall fracture with a posterior dislocation of the hip.
Posterior wall fracture with a posterior dislocation of the hip.
 Posterior wall fracture preoperative obturator view.
Posterior wall fracture preoperative obturator view.
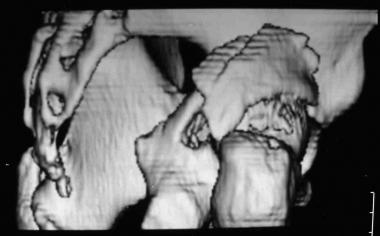 Three-dimensional (3-D) CT scan showing a posterior wall fracture.
Three-dimensional (3-D) CT scan showing a posterior wall fracture.
Extended posterior-wall fractures can involve the entire retroacetabular surface and include a portion of the greater or lesser sciatic notch, the ischial tuberosity, or both. The ilioischial line, however, remains intact on the anteroposterior (AP) view.
Posteriocolumn fractures include only the ischial portion of the bone. The entire retroacetabular surface is displaced with the posterior column. As the vertical line separating the anterior column from the posterior column traverses inferiorly, it most commonly enters the obturator foramen. An associated fracture of the inferior pubic ramus is present.
Sometimes, the fracture line traverses just posterior to the obturator foramen, splitting the ischial tuberosity. The ilioischial line typically is displaced and disassociated from the teardrop. However, when a large portion of the quadrilateral surface remains intact with the posterior column, the teardrop and a portion of the pelvic brim displace with the posterior column.
Anterior-wall fractures (see the images below) are uncommon injuries and often occur in conjunction with anterior dislocations.
 Anterior wall fracture.
Anterior wall fracture.
 Anterior wall fracture: Three-dimensional reconstruction.
Anterior wall fracture: Three-dimensional reconstruction.
Low anterior-column fractures involve only the superior ramus and pubic portion of the acetabulum. High anterior-column fractures can involve the entire anterior border of the innominate bone. The pelvic brim and iliopectineal line are displaced. Medial translation of the entire roof or a portion of the roof is typical of displacement of a high or intermediate anterior-column fracture.
Transverse fractures (see the image below) divide the innominate bone into two portions. A horizontally displaced fracture line crosses the acetabulum at a variable level. The innominate bone is then divided into a superior part and a lower part. The superior part is composed of the iliac wing and a portion of the roof of the acetabulum. The lower part of the bone, the ischiopubic segment, is composed of an intact obturator foramen with the anterior and posterior walls of the acetabulum.
 Transverse fracture.
Transverse fracture.
Letournel further divided transverse fractures into the following three subtypes:
Fracture patterns
Associated acetabulum fracture patterns are the more complicated fracture patterns and include the following:
Anterior with posterior hemitransverse fractures combine an anterior-wall or anterior-column fracture with a horizontal transverse component, which traverses the posterior column at a low level. The distinction between the associated anterior-column and associated posterior hemitransverse and T-shaped patterns is often subtle. In the anterior plus posterior hemitransverse fracture, the anterior component typically is at a higher level and is more displaced than the posterior component.
The posterior-column with posterior-wall pattern (see the images below) divides the posterior column into a larger posterior-column component and an associated posterior-wall component. The ilioischial line typically is displaced and disassociated from the teardrop.
 Posterior lip with posterior column injury, anteroposterior view.
Posterior lip with posterior column injury, anteroposterior view.
 Posterior wall with posterior column fracture, 3-D reconstruction.
Posterior wall with posterior column fracture, 3-D reconstruction.
The transverse with posterior-wall pattern (see the image below) combines a normal transverse configuration with one or more separate posterior-wall fragments. A fracture of the inferior pubic ramus typically is not seen.
 Transverse with posterior lip fracture.
Transverse with posterior lip fracture.
A T-shaped fracture (see the images below) is similar to a transverse fracture except for the addition of a vertical split along the quadrilateral surface and acetabular fossa (the stem of the T), which divides the anterior column from the posterior column. An associated fracture of the inferior pubic ramus typically is present.
 T-shaped fracture (break in the margins of the obturator foramen).
T-shaped fracture (break in the margins of the obturator foramen).
 T-shaped fracture, obturator view.
T-shaped fracture, obturator view.
In both-column fractures (see the images below), the anterior and posterior columns are separated from each other, and all articular segments are detached from the intact portion of the posterior ilium, which remains attached to the sacrum. A fracture of both columns is associated with the spur sign, in which the fractured edge of the intact posterior iliac wing is seen prominently relative to the medially displaced articular segments on the obturator oblique radiographic view. This sign is pathognomonic of an injury to both columns.
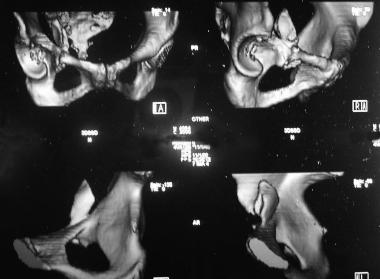
 Both-column fracture, 3-D reconstruction, anteroposterior view.
Both-column fracture, 3-D reconstruction, anteroposterior view.
 Both-column fracture, 3-D reconstruction, iliac view.
Both-column fracture, 3-D reconstruction, iliac view.
 Both-column fracture, 3-D reconstruction, obturator view.
Both-column fracture, 3-D reconstruction, obturator view.
AO-ASIF classification
The Arbeitsgemeinschaft für Osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) classification is more comprehensive and is shown in the image below. This can be simplified as follows:
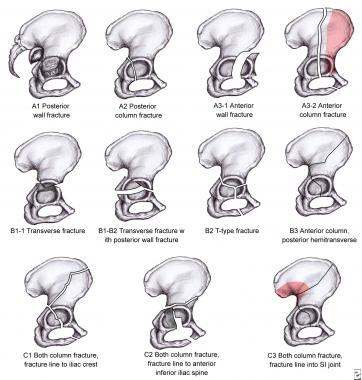 The Arbeitsgemeinschaft fur osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) classification.
The Arbeitsgemeinschaft fur osteosynthesefragen–Association for the Study of Internal Fixation (AO-ASIF) classification.
Pediatric acetabular fractures
Pediatric acetabular fractures are classified as follows:
Pediatric acetabular fractures are important, in that the triradiate cartilage remains open until the age of approximately 12 years. Therefore, if the acetabulum is injured before its closure, growth arrest may result, leading to a shallow acetabulum and progressive subluxation of the hip.[7] Conversely, in patients older than 12 years, the chance of significant growth disturbance is minimal.
Bucholz et al recognized two main types of physeal disturbances with triradiate cartilage injuries, as follows[8] :
Dora et al monitored 10 patients with posttraumatic acetabular dysplasia and reported that all 10 patients demonstrated marked retroversion averaging 27°, whereas the contralateral acetabuli showed 23° of anteversion; the average center-edge angle was 9.5°.[9] The hip joint typically was in a lateral and caudal position, and a significant posterolateral deficiency was present.
The exact incidence of acetabular fractures in various parts of the world is not known. Studies at level I trauma centers have shown an admission rate for pelvic and acetabular fractures of 0.5-7.5% (see Table 1 below).
Table 1. Relative Frequency of Acetabular Fracture Types in Various Studies (Open Table in a new window)
Fracture type Letournel, [3] %Peltier reported an incidence of 24% acetabular fractures in his series of adult pelvic fractures.[12] Reed documented that approximately 5-10% of pediatric pelvic injuries involve the acetabulum.[13]
Factors in the injury pattern affecting prognosis include the following:
Treatment factors affecting the prognosis are the quality of the reduction, which ideally restores congruity, and the quality of fixation, which ideally restores stability.[14]
The prognosis can also be affected by complications such as the following:
Studies have confirmed the positive association between the accuracy of reduction and a better long-term result.[10, 15] However, many series have shown that even when these goals are achieved, posttraumatic arthritis still occurs in as many as 30% of patients.[4, 10, 16, 17, 18] Contributing factors may include the following:
Once symptomatic posttraumatic arthritis has developed, options for salvage generally are limited to total hip arthroplasty and arthrodesis.
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved