

Arthropathy and resulting arthritis of the wrist give rise to pain, which in turn leads to disability and decreased function of the upper extremity.[1] The articulation afforded the hand by the wrist is important for mobility, strength, and dexterity. The pain produced by arthropathy of the wrist causes the patient to use a wrist splint to decrease pain. However, loss of mobility due to splinting is only part of the problem. The pull of the finger and wrist flexors and extensors exerts considerable force on the many intercarpal joints. Pain produced by bone-on-bone contact is compounded by the pressure exerted in active motion, and the result is reluctance of the patient to perform active motion.
Joint arthropathy resulting in wrist arthritis is nearly identical to arthropathy in other joints, including the hip and knee. The principal problem is loss of articular cartilage between the carpal bones and/or the metacarpal and distal radius. The major difference is the fact that the wrist is not normally a weightbearing joint.
Causative factors for wrist arthropathy include, but are not limited to, the following:
Wrist arthrodesis is also indicated for stabilization of the wrist when combined with tendon transfers, correction of wrist deformities in patients with spastic hemiplegia, and for salvage of unsuccessful wrist arthroplasty.
The various etiologies notwithstanding, the common pathway of disease includes the following:
Bone-on-bone contact produces reactive bone formation in the subchondral area and eventually results in eburnation (sclerosis) of the contacting bone surfaces. Pressure and abrasion irritate afferent nerves in the substance of the bone. Inflammation is either a result of the primary etiology (eg, rheumatoid arthritis, gout) or can be a result of synovial irritation. Prostaglandins and cytokines are generated as a result of inflammation, causing pain and decreased mobility of the wrist.
No comprehensive epidemiology data for wrist arthropathy are reported in the literature. However, Watson and Ballet reviewed 4000 wrist radiographs for evidence of arthritis (eg, joint space narrowing, osteophyte formation, subchondral reactive bone formation, subchondral cyst formation).[2] Of these 4000 radiographs, 210 (5.3%) had unequivocal radiographic changes consistent with wrist arthritis. The scapholunate advanced collapse (SLAC) pattern was most prevalent, noted in 120 (57% of pathologic joints) of the 210 radiographs.
Triscaphoid arthritis (ie, scaphoid, trapezoid, trapezium) was found in 14% of affected wrists.[2] Nonscaphoid-related arthritis was found in only 3% of affected wrists. The radiolunate joint was almost never affected. Note that this population did not include wrist arthritis due to inflammatory arthropathy.
The goal of arthrodesis for painful arthritis is to prevent motion by obtaining bony consolidation of worn joint surfaces and thereby remove the pain generated in the joint. In addition, wrist arthrodesis can be beneficial in providing a more functional hand and upper extremity in patients with deforming spastic hemiplegia.
The earliest wrist arthrodesis procedures consisted of decortication and combinations of corticocancellous bone grafts keyed into accurately cut slots and keyways. Immobilization of the wrist was required postoperatively to ensure adequate healing. Later, the use of percutaneous pin fixation allowed for decreased reliance on external immobilization. Steinmann pins were also employed as internal splints in an attempt to provide more rigid fixation. The development of internal fixation with plates and screws revolutionized wrist arthrodesis and almost completely eliminated the need for external immobilization.[3]
Currently, state-of-the-art total wrist arthrodesis employs the use of a specifically designed dynamic compression plate, which allows rigid fixation with larger screws proximally and smaller screws distally to reduce the risk of fracturing the metacarpals. Limited intercarpal arthrodeses still employ combinations of Kirschner wires (K-wires), screws, staples, and structural bone grafting. Specialty plate and screw constructs have been designed for use in both limited and total arthrodesis of the wrist.[4]
NextArthrodesis of the wrist joint is indicated in degenerative joint disease and instability associated with restricted and painful range of motion. Further indications are unsuccessful reconstruction, partial arthrodesis, or arthroplasty, with or without total joint replacement. Total wrist fusion still represents the main treatment for severe posttraumatic disorders of the wrist due to long-standing scaphoid nonunion advanced collapse (SNAC), SLAC (see the images below), and occasionally posttraumatic arthritis secondary to distal radius fractures.
 Wrist arthrodesis. Stage III scapholunate advanced collapse (SLAC) wrist. Patient desired motion-preserving procedure.
Wrist arthrodesis. Stage III scapholunate advanced collapse (SLAC) wrist. Patient desired motion-preserving procedure.
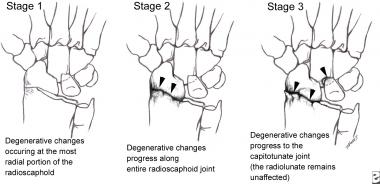 Wrist arthrodesis. Sequence of degenerative changes in scapholunate advanced collapse (SLAC) wrist arthritis pattern.
Wrist arthrodesis. Sequence of degenerative changes in scapholunate advanced collapse (SLAC) wrist arthritis pattern.
Specific indications for radiocarpal arthrodesis include the following:
Midcarpal fusion has become increasingly more popular because it preserves motion. However, whether the preserved motion is of real benefit from the patient's point of view is questionable, because complete pain relief is rare following this type of limited wrist fusion. Midcarpal fusion is preferable to total wrist fusion for treatment of progressive carpal collapse (eg, SLAC, SNAC).[6, 7] Currently, patients with either occupations or interests that require intricate use of their hands are believed to have better outcomes with limited arthrodeses because of the preservation of motion.[8]
Subtotal arthrodesis is not recommended for patients with rheumatoid wrist joints or those engaged in hard manual labor, because the functional results are only negligibly better than those obtained with total arthrodesis. Limited wrist arthrodesis is the surgical fusion of selected bones of the wrist. In each case, the extent of the fusion is determined by the extent of the disease process.
Limited wrist arthrodesis is an alternative to complete wrist fusion when a localized area of degenerative change or instability in the carpus is present. It relieves pain, yet it still allows some range of motion.[9] Biomechanical alterations do occur following limited intracarpal fusions. Subtotal arthrodeses of the wrist are indicated for painful arthritis involving one or two radiocarpal or intracarpal joint surfaces, stabilization of carpal collapse deformities, failed ligament reconstructions or repairs, or bone tumors with partial carpal involvement.[10]
Limited wrist arthrodesis is a useful method for treating specific carpal disorders that maximizes residual wrist motion and strength while attempting to eliminate pain. Selective fusion of specific carpal bones can be used in persons with degenerative arthritis, rotatory subluxation of the scaphoid, midcarpal instability, scaphoid nonunion, Kienböck disease, and congenital synchondrosis or partial fusion of specific carpal joints.[11]
The need for fusion of the capitate, lunate, triquetrum, and hamate is still unclear. Evidence suggests that there may be an improved ability to reduce the capitate on the lunate and a lower rate of nonunion when the triquetrum and scaphoid are excised and the only fusion surfaces are localized between the capitate and lunate. Migration of the screws can be an issue with this technique.[12, 13]
A contraindication to wrist arthrodesis is an open distal radial physis. Severe trauma to the wrist and physis might require epiphysiodesis and, therefore, allow for fusion. A relative contraindication is an elderly patient with a sedentary lifestyle, especially if the targeted wrist is the nondominant wrist. In this situation, an arthroplasty may be more suitable. Other contraindications include the following:
One surgical treatment not involving arthrodesis is particularly useful in the SLAC wrist. The treatment involves partial denervation of the wrist through division of the anterior and posterior interosseous nerves at the level of the wrist through a small dorsal incision, as described by Berger.[14] This does not affect the articular changes directly but can reduce symptoms to allow arthrodesis to be postponed or avoided.
The surgical technique depends mainly on the quality of bone substance and degree of joint degeneration. Differences between fusion types include the type of bone graft and osteosynthesis being used. The aim is to create a stable joint in an acceptable functional position. The position of arthrodesis depends on the patient's needs. A neutral position is generally accepted in patients with rheumatoid arthritis, whereas slight wrist extension and ulnar deviation are preferred in patients with degenerative joint disease.[15, 16, 17, 18] A stable osteosynthesis with plate fixation is reliable and allows early rehabilitation.
The use of internal fixation has decreased the need for prolonged immobilization in a cast postoperatively and has improved outcomes. Historically, single or multiple screws have been used to hold a cortical bone graft in place in the dorsal aspect of the wrist. The use of a single K-wire to supplement immobilization in a cast has also been described. A technique described for use in patients with rheumatoid arthritis uses a single permanent Steinmann pin advanced retrograde from the third metacarpal into the medullary canal of the radius.
A later modification of this method was the addition of a Rush rod with supplementary staple fixation, eliminating the need for postoperative immobilization in a cast. In fact, the results of a modification of this technique reported by Millender and Nalebuff support the finding that immobilization in a plaster cast is not imperative after wrist arthrodesis in patients with rheumatoid arthritis when internal fixation is used.[19] This technique has also been used for arthrodesis of wrists in individuals with posttraumatic disorders.
Other methods of internal fixation included the use of multiple staples without an intramedullary pin and the technique of placing a pin from the thenar eminence into the medullary canal of the radius without exposing the wrist.
The use of dorsal placement of a nine-hole plate from the second metacarpal to the radius with an additional corticocancellous autogenous iliac crest bone graft was first described in 1972. Later, Larsson described a similar technique that used a six-hole self-compressing plate.[20] By the early 1980s, a larger eight-hole 3.5-mm dynamic compression plate was advocated to provide more appropriate rigid fixation.
Currently, a specifically designed wrist arthrodesis plate is available, which combines a 3.5-mm dynamic compression plate proximally and a 2.7-mm dynamic compression plate distally. (See Technique.) This combination AO/ASIF (Arbeitsgemeinschaft für Osteosynthesefragen/Association for the Study of Internal Fixation) wrist arthrodesis plate allows for improved and stable fixation by using larger screws in the distal radius and provides reduced risk of metacarpal fracture and fragmentation by using smaller 2.7-mm screws into the metacarpal.
Use of this wrist fusion plate yields a high rate of fusion when bone graft is used and, in comparison to other wrist arthrodesis techniques, yields a more predictable rate of fusion.[21] Three versions of the AO/ASIF wrist fusion plate are available: short carpal bend, long carpal bend, and straight plate. All versions use three 2.7-mm metacarpal screws, one 2.7-mm capitate screw, and four 3.5-mm radius screws.
The use of corticocancellous bone graft from the iliac crest is still advocated to augment the site of the arthrodesis for appropriate osseous consolidation. Slot grafts and onlay grafts create the added physical integrity of corticocancellous grafts. However, data have been reported showing that cancellous bone alone is sufficient for fusion when used with fixation. This has facilitated harvesting cancellous bone from the distal radius, eliminating the need for iliac crest bone graft harvest when limited amounts of graft are needed.
The performance of proximal row carpectomy in conjunction with total wrist arthrodesis in patients with rheumatoid arthritis has been described, with a view to simplifying the arthrodesis and rendering an iliac bone graft unnecessary. In a study by Pham et al, the combination of total wrist arthrodesis with proximal row carpectomy was reliably and reproducibly beneficial, and no adverse effects related to loss of carpal height were reported.[22]
Limited intercarpal arthrodesis can be achieved by either onlay corticocancellous grafts or interpositional cancellous grafts performed through a dorsal exposure. In an attempt to preserve motion, various limited arthrodeses of the carpus have been described. Although these procedures are technically demanding, successful results may be expected, especially in conditions of carpal instability.
The decision as to which carpal bones are to be fused depends on the location and type of pathology. Kienböck disease (AVN of the lunate) can be treated by fusing the radial aspect of the carpus. A scaphotrapeziotrapezoidal (STT) arthrodesis stabilizes the carpus and unloads the central column of the wrist.[23] Scapholunate dissociation resulting from rupture of the scapholunate ligament can also be treated with STT fusion.
If degenerative changes are evident in the radioscaphoid articulation, then a scaphoid excision and a four-corner (ie, lunate-triquetrum-capitate-hamate) arthrodesis is necessary.[24, 25, 26, 27, 12] It has been suggested that capitolunate arthrodesis may be an alternative to four-corner fusion for SNAC wrists with osteoarthritis.[13]
Wrist arthrodesis results in a high degree of patient satisfaction with respect to pain relief and correction of deformity.[28] Patients are able to accomplish most daily tasks and activities by learning to adapt to and compensate for the loss of wrist motion. After wrist arthrodesis, patients adapt to their fused wrists but still have difficulty with some activities, such as getting the hand into tight places, heavy lifting, and positioning the hand for some specific activities. However, satisfactory postoperative function appears to depend more on pain relief than on residual motion.[29]
Wrist arthrodesis, either pancarpal or limited, is considered the primary surgical alternative in patients with most end-stage arthritic conditions of the wrist. The pancarpal arthrodesis is a predictable durable alternative to a variety of posttraumatic, degenerative, or neoplastic conditions of the wrist. However, some authors report that complications may be prevalent. This procedure may also be modified and applied to the destroyed rheumatoid wrist.
Overall, selection of fixation mode depends on bone quality.[30] With the current wide array of surgical alternatives, the surgeon must consider each case carefully and select the procedure that best applies to each particular situation. Furthermore, the surgeon must educate the patient on the limitations of each procedure.
Solid fusion, pain relief, and satisfactory functional results can be achieved after wrist arthrodesis. Prerequisites for obtaining such results are as follows[31] :
Copyright © www.orthopaedics.win Bone Health All Rights Reserved