

Carpal ligament instability is defined as any malalignment of the carpus. This may be evident on plain radiography as a static deformity; alternatively, the situation may be a dynamic one, which becomes evident only when external forces are placed on the wrist. The malalignment may appear after a single traumatic event or may be secondary to chronic attenuation of supporting ligaments after a traumatic event or secondary to an underlying disease process (eg, rheumatoid arthritis,pseudogout).
The human wrist joint is a complex arrangement of small bones and ligaments that form a mobile yet stable link from the powerful forearm to the hand. The normally functioning carpus can position the hand precisely relative to the forearm and provides remarkably stable transmission of forces. Motion and stability of the carpus provide the critical foundation for maximum hand function from precise fine motor control to power grip activities.
When the normal mechanics of the wrist are disrupted, the instability of the carpal bones results in weakness, stiffness, chronic pain, and often arthritis if not treated appropriately. Although the early clinical and radiographic findings may be subtle, an understanding of wrist kinematics and instability patterns can facilitate early diagnosis and management. Unfortunately, selecting the optimal treatment remains a difficult judgment in most cases.
Linscheid et al described traumatic carpal instability in 1972.[1] Since the early reports, anatomic and biomechanical studies have provided a foundation for understanding carpal motion, stresses, and pathologic instability.[2, 3] Building on these studies, various models have been suggested to explain the remarkable strength and mobility of this complex joint and the predictable patterns of failure.
This article presents the current understanding of pathologic carpal instability, the common classification patterns, and early treatment options that may avoid protracted dysfunction. Appropriate hand therapy is essential to maximize recovery but requires an appreciation of the limitations of carpal instability dysfunction and the goals of various treatment options.
NextThe wrist contains eight carpal bones. Anatomically and functionally, these bones are divided into proximal and distal rows. The proximal row is formed by the scaphoid, the lunate, and the triquetrum. Although the pisiform is anatomically located on the palmar surface of the proximal row, it is a sesamoid bone within the flexor carpi ulnaris tendon; it does not contribute to the kinematics of the proximal row. The trapezium, the trapezoid, the capitate, and the hamate form the distal row.
Multiple ligaments help stabilize the wrist to the forearm and hand. Extrinsic ligaments span the radiocarpal joint, whereas intrinsic ligaments form connections between individual carpal bones.
Extrinsic
An important extrinsic ligament on the dorsal aspect of the wrist is the dorsal radiocarpal ligament (see the first image below). This ligament originates on the radius and has minor attachments to the lunate, with the bulk of the attachment on the triquetrum. There are many more extrinsic ligaments on the volar aspect of the wrist. From radial to ulnar, they include the radioscaphocapitate, radioscapholunate, short radiolunate, long radiolunate, ulnolunate, and ulnotriquetrum ligaments (see the second image below).
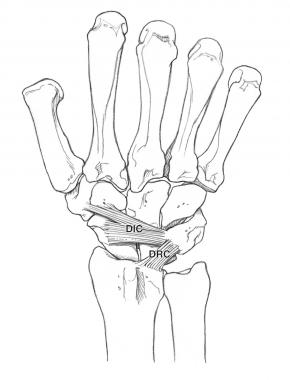 (Click image to enlarge.) Dorsal carpal ligaments. Copyright Mayo Clinic, used with permission of Mayo Foundation.
(Click image to enlarge.) Dorsal carpal ligaments. Copyright Mayo Clinic, used with permission of Mayo Foundation.
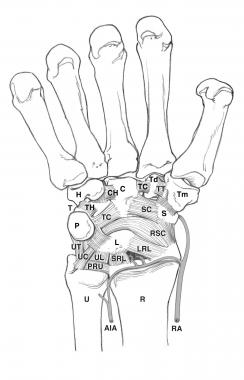 (Click image to enlarge.) Volar carpal ligaments. Copyright Mayo Clinic, used with permission of the Mayo Foundation.
(Click image to enlarge.) Volar carpal ligaments. Copyright Mayo Clinic, used with permission of the Mayo Foundation.
Intrinsic
The intrinsic ligaments are stout structures that originate and insert within the carpus. The two most important intrinsic ligaments include the scapholunate interosseous ligament (SLIL) and the lunotriquetral interosseous ligament (LTIL). The SLIL, which joins the scaphoid and the lunate, is probably one of the most important ligaments in the wrist. Injury of the SLIL can result in one of most common causes of carpal instability: scapholunate dissociation.
The SLIL is a C-shaped ligament that is divided into three separate components, as follows[4] :
The LTIL connects the lunate and triquetrum. Like the SLIL, the LTIL is C-shaped and has three separate components. Unlike the SLIL, it has a palmar component that is stouter than its volar component.
Two intrinsic ligaments that cross from the proximal row to the distal row are the scaphocapitate ligament and the dorsal intercarpal ligament. The scaphocapitate ligament crosses the volar midcarpal joint and attaches from the distal pole of the scaphoid to the body of the capitate. Across the dorsal midcarpal joint, the dorsal intercarpal ligament originates from the triquetrum, attaches to the scaphoid dorsal ridge, and then inserts into the dorsal distal third of the scaphoid and to the scaphoid-trapezium ligament.
Over the past several decades, many theoretical models have been described to explain the complexities of carpal motion. The column theory, first proposed by Navarro in 1935,[5] recognized some motion between the bones of the proximal row and divided the wrist into the following three columns:
Although this theory does not explain the coupled motions that occur within the proximal and distal rows, it does help explain the load patterns seen through the wrist.
The row theory of carpal kinematics is based on the observation that the proximal and distal rows work as two separate functional units. Gilford et al expanded on this theory by noting that flexion-extension motions of the wrist are accomplished by relatively equal contributions from the radiolunate and lunocapitate joints, and they proposed that each row rotates around a single center of rotation near its proximal articular surface (see the image below).[6]
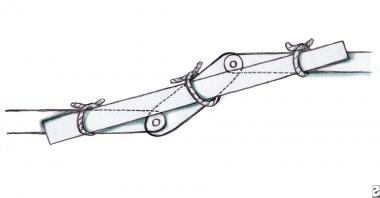 The scaphoid acts like a bridge between the proximal and distal row and protects the link from collapsing.
The scaphoid acts like a bridge between the proximal and distal row and protects the link from collapsing.
Gilford et al also emphasized the instability of such a two-link system under load and the tendency for the system to crumple without a stabilizing mechanism.[6] They believed that the scaphoid should be considered part of both rows and underscored its importance as a bridge, or tie rod, to stabilize an otherwise unstable arrangement (see the image below).
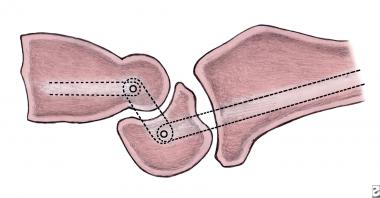 The wrist is a simple link between the proximal and distal rows. The pivot point is at the center of rotation of the capitate and lunate. This joint, without other supporting structures, is stable only in tension. It is unstable in compression, as this figure depicts, and tends to collapse.
The wrist is a simple link between the proximal and distal rows. The pivot point is at the center of rotation of the capitate and lunate. This joint, without other supporting structures, is stable only in tension. It is unstable in compression, as this figure depicts, and tends to collapse.
Because no tendons insert on the scaphoid, lunate, and triquetrum, in 1972 Linscheid et al considered the scaphoid, lunate, and capitate to be an intercalated segment interposed between the articular surfaces of the radius and ulna and the rigidly bound distal carpal row.[1]
Muscle contractions impart rotational moments to the proximal row through the distal row, and carpal motion is governed by a combination of ligamentous and articular constraints. The strong interosseous ligaments between the three proximal carpal bones enable them to move in a synchronized fashion during wrist motion. The scaphoid, lunate, and triquetrum rotate in the same primary direction, albeit to different magnitudes, during any motion of the hand.
A specific example of this interaction may be observed during radial-ulnar deviation. As the wrist deviates ulnarly, the entire proximal row extends. Conversely, as the wrist deviates radially, the entire proximal row flexes. Although the mechanism by which this occurs has not been fully elucidated, most authors believe that this motion is a result of a combination of ligamentous constraints and carpal articular geometry between the proximal intercalated row and the distal row.
A theory proposed by Linscheid and Dobyns in 1989 is that the distal pole of the scaphoid flexes because of pressure by the trapezium and trapezoid during radial deviation.[7] The rest of the proximal row then flexes because of the strong interosseous ligaments connecting the lunate to the scaphoid and the triquetrum to the lunate.
In another theory, Weber proposed that the unique helicoidal shape of the triquetrohamate articulation forces the distal row to translate dorsally and the triquetrum to tilt into extension as the wrist deviates ulnarly.[8] Dorsal translation of the distal row contributes to an extension moment on the proximal row. The opposite occurs during radial deviation with palmarly directed force on the proximal row, causing flexion.
Some have theorized that an individual's carpal kinematic behavior can be explained by some combination of the columnar theory with the row theory.
Craigen and Stanley analyzed radiographs of 52 normal wrists and found that from ulnar deviation to radial deviation, the amount of scaphoid shortening and ulnar translation of the scaphoid varies in a normal distribution.[9] If the scaphoid shortens more, it translates less. By their interpretation, a column-type wrist shows greater shortening. They also found that females were more likely to have greater scaphoid shortening and less translation.
This individual variation in kinematic behavior was also supported by Garcia-Elias et al, who attributed it to individual variation in laxity.[10] They examined 60 healthy volunteers and found that physiologic differences in wrist ligamentous laxity affected carpal kinematics. In radial-ulnar deviation, the scaphoid of very lax wrists moved preferentially in the sagittal plane (flexion-extension), whereas in the more rigid wrists, the scaphoid moved preferentially in the frontal plane (radioulnar deviation).
The oval-ring theory functionally depicts the carpus as a transverse ring formed by proximal and distal rows and joined by two physiologic links, one radial and the other ulnar.[11] The radial link is the mobile scaphotrapezial joint, and the ulnar link is the rotatory triquetrohamate joint.
Carpal ligament instability results from an injury to one or more ligamentous or bony constraints in the wrist. Depending on the force, rate, and point of impact and on the position of the wrist, a fall on an outstretched wrist can result in a range of injuries, including the following:
This type of trauma can also result in injury to one or more ligamentous structures in the wrist, causing carpal instability. Perilunate instability is described as progressing from the scapholunate and the capitolunate to the lunotriquetral joint.
Using a cadaveric trauma model, Mayfield et al observed progressive injury patterns when the wrist was loaded in extension, ulnar deviation, and carpal supination.[12] This perilunar instability is divided into the following four stages (see the image below):
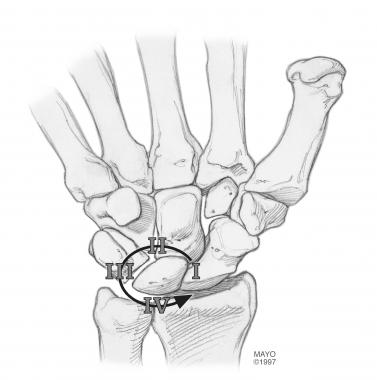 Mayfield perilunate instability pattern. Copyright Mayo Clinic, used with permission of the Mayo Foundation.
Mayfield perilunate instability pattern. Copyright Mayo Clinic, used with permission of the Mayo Foundation.
However, if the carpus is pronated and the hypothenar area is struck first, an ulnar traumatic pattern may be observed. Specifically, disruption of the ulnotriquetral ligament complex and the LTIL occurs.[13] As the triquetrum no longer holds the lunate, it falls into a flexed position because of pressure from the capitate and its connection with the scaphoid. With attenuation or injury to the dorsal intercarpal ligament, a volar intercalated-segment instability (VISI) pattern ensues; this can be visualized on lateral radiography. An LTIL tear most commonly results in a VISI deformity.
In addition to a direct loading type of trauma, rotational force to the wrist can also result in ligamentous injuries, eg, the forces that occur when holding a power drill while the drill bit is jammed. This type of trauma can result in injuries to the LTIL and ulnotriquetral ligament complex and result in the lunotriquetral instability.[14]
Some instability patterns arise after chronic attrition of supporting ligaments. One traumatic event may result in some subtle ligamentous injury but no clear instability initially. However, over time, continued normal daily loading of the wrist can result in symptomatic instability. An example is seen with scaphoid fractures, where a dorsal intercalated-segment instability DISI deformity tends to appear late after the initial traumatic event.
Supporting ligaments can also be important in preventing carpal instability in the presence of other significant ligamentous injury. For example, many cadaveric studies have shown that isolated sectioning of the SLIL does not result in a frank radiographic scapholunate gap or dissociation.
In 1986, Johnson and Carrera described a midcarpal instability in which the capitate dorsally subluxates out of the cup of the lunate during a fluoroscopic dorsal-displacement stress test.[15] This is associated with a painful snap or click that reproduces the patient's symptoms. They attributed the cause of this instability to attenuation of the radioscaphocapitate ligament after prior trauma.
In 1975, Dobyns et al reviewed their experience and found that 10% of all carpal injuries resulted in instability.[16]
In 1988, Jones evaluated 100 consecutive patients with wrist sprains by using dynamic radiography (clenched-fist views) and found that 19 had an increased scapholunate gap.[17]
The incidence of carpal instability that is associated with other specific fractures is relatively high. Reviewing 134 distal radius fractures, Tang in 1992 found radiographic evidence of carpal instability in 30% of the cases.[18]
Geissler and Freedland prospectively reviewed 60 displaced intra-articular distal radius fractures that were being treated with arthroscopy-assisted reduction and internal fixation.[19] They found that 43% had concomitant tears in the fibrocartilage complex and 32% also had tears in the scapholunate ligament.
Weber reviewed 36 patients with acute scaphoid waist fractures and found that 28% had a DISI deformity.[20]
Clinical Presentation
Copyright © www.orthopaedics.win Bone Health All Rights Reserved