

The term floating elbow was first introduced by Stanitski and Micheli to describe an injury pattern in children involving concomitant fractures of the forearm axis and supracondylar humerus in the same extremity (see first image below).[1] This description has been extended to adult patients who sustain ipsilateral fractures of the humerus and forearm (see second image below).[2]
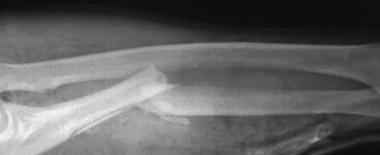 Grade IIIA open ulna fracture in a motorcyclist with associated radial head humeral injuries.
Grade IIIA open ulna fracture in a motorcyclist with associated radial head humeral injuries.
 Close-up of radial head dislocation with evidence of air in soft tissues.
Close-up of radial head dislocation with evidence of air in soft tissues.
The spectrum of injury can vary greatly, depending on the force dissipated by the extremity and its position in space at the time of the incident. The nature of treatment of these injuries is dictated somewhat by the condition of the soft tissues and neurovascular bundle in the affected extremity and by other pending medical and surgical issues. As the orthopedic community has grown to understand how to best treat the isolated humerus and forearm fracture, this knowledge has been used to improve the outcome of these combined complex upper extremity injuries.[3, 4, 5]
NextFloating elbow is an injury pattern involving a fracture of the humerus and a fracture of both the radius and the ulna in the same extremity. This injury may be associated with an elbow dislocation in patients who sustain high-energy injuries (see image below). The location of the fracture may dictate the treatment options. Regardless of where the fracture occurs, if the elbow remains dissociated from the hand and shoulder, the fracture is deemed to be floating.
 Ipsilateral segmental humeral fracture.
Ipsilateral segmental humeral fracture.
Fractures of the humerus associated with fractures of the forearm are rare, both in adults and in children. Most of these injuries in adults are the result of high-energy injuries.[6] The literature has only a handful of reports describing the injury and results of treatment. In children, the incidence is better known, cited at 2-13% for concomitant fractures of the forearm axis and supracondylar humerus.[7, 8, 9, 10, 11]
The likely mechanism of injury in children who sustain an injury to the distal forearm axis and supracondylar humerus is a fall on the outstretched arm with the forearm pronated and the wrist hyperextended.[7, 8, 9, 10] Direct trauma and other positions of the arm and forearm in space after falls also can cause similar constellations of injuries. In adult patients, the usual mechanism is direct high-velocity trauma, such as sideswipe injuries, crush-type injuries, or falls from extreme heights.[2, 12]
Patients with a floating elbow report pain and have an obvious deformity in the affected extremity. In both adults and children, the occurrence of neurovascular deficit ranges from 25-45%. Other soft-tissue and associated injuries (eg, open fractures, closed head injuries [CHIs], thoracoabdominal trauma) depend on the mechanism of injury and severity of pathology.
A thorough physical examination is the benchmark of the initial patient evaluation. Careful documentation of the neurovascular status of the injured limb is crucial. Patients with a persistent pulseless extremity despite fracture reduction should undergo arteriography to rule out vascular injury if a delay in operative intervention is anticipated. Evaluation of soft-tissue viability is important in patients who sustain crush injuries and open fractures. The development of compartment syndrome should be diligently determined and appropriately treated.[13] All fractures should be reduced and splinted as appropriate.
Indications for treatment of isolated humerus and forearm fractures vary greatly with patient age, location of the fracture, and injury to the soft-tissue envelope.[14, 15] However, the rules change when these fractures occur concomitantly in the same extremity. While reports are few in adults, available data suggest that patients with multiple fractures in the same upper extremity fare better with anatomic reduction and some type of definitive fixation both for humerus and for forearm fractures. In children, reduction with percutaneous pinning is the standard of care for the supracondylar humerus fracture component, and management of the forearm component has been shown to be managed successfully either with closed or percutaneous techniques with similar results. Appropriate soft-tissue management is crucial to aid in fracture healing and may dictate the type of fixation used.[16, 17, 18, 19, 20, 21, 22]
The landmarks for the humerus include the greater and lesser tuberosities, the deltoid tubercle, and the epicondyles distally. Proximally, the surgical and anatomic neck can define the humerus. The shaft of the humerus has 2 distinct grooves, proximally between the 2 tuberosities for the biceps tendon and posteriorly in the midportion for the radial nerve. As the shaft flares distally, the humerus broadens out into its medial and lateral epicondyles. These 2 epicondyles act as columns and support the trochlea of the distal humerus. The lateral column includes the epicondyle and ends in the radial articulation of the capitellum. The spool-like trochlea is suspended between the 2 epicondyles and lies in 4-8° of valgus and internal rotation with respect to the humeral shaft. The rotational axis of the capitellum lies 12-15 mm anterior to the anterior humeral line, in line with the axis of rotation of the trochlea.[23, 24]
A thin shell of bone separates the coronoid and olecranon fossae just proximal to the trochlea. The olecranon is the flared proximal portion of the ulna. It articulates with the trochlea at its semilunar notch. The ulnar contribution to the proximal radioulnar joint lies just lateral to the coronoid process, the radial notch. The proximal radius is composed of a concave disc-shaped radial head and a short narrow neck. The ulnohumeral articulation is characterized as a hinge/ginglymus joint with 1 º of freedom (flexion/extension). Its stability is enhanced by the congruence of the articular surfaces, as well as by the medial collateral and lateral ulnar collateral ligaments. The radiohumeral articulation functions as a pivot, allowing flexion, extension, and rotation. It is stabilized by the lateral collateral ligament and the annular ligament.
The forearm is composed of the radius and ulna. Just distal to the radial head, the bicipital tuberosity lies on the anteromedial surface of the radial neck. The radius has a bow with an anterolateral convexity. This is important in that it must be restored to allow for normal rotation about the forearm axis. The distal radius flares at the metaphysis to form a broad articulation with the scaphoid and lunate, with the radial styloid at the lateral margin of the distal articular surface. The Lister tubercle is palpable on the dorsal surface of the distal radius and is palpable between the extensor carpi radialis longus and brevis and the extensor pollicis tendons. The ulna is triangular. It narrows and terminates in the distal ulnar head and styloid.
The brachial musculature can be divided into flexor and extensor compartments. The flexor muscles include the biceps, brachialis, and coracobrachialis. The extensor compartment consists of the triceps with its medial, lateral, and long heads. The medial epicondyle acts as the origin of the forearm flexor muscles: the flexor carpi radialis, flexor carpi ulnaris (FCU), flexor digitorum superficialis (FDS), and palmaris longus (when present). The lateral epicondyle provides the origin for the extensor muscles: the extensor carpi radialis longus and brevis, extensor carpi ulnaris, extensor digiti minimi, and the supinator and anconeus muscles.
The forearm is divided into 3 compartments: the volar compartment (pronator teres and quadratus, flexor carpi radialis and FCU, FDS and flexor digitorum profundus [FDP], and flexor pollicis longus [FPL] with FDP and FPL, considered by some to be a separate, deep compartment); the mobile wad (extensor carpi radialis longus and brevis and the brachioradialis); and the dorsal compartment (extensor digitorum, extensor digiti minimi, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis).
The axillary artery becomes the brachial artery as it passes underneath the pectoralis minor tendon. It then runs medially with the median nerve underneath the biceps brachii muscle. The profunda brachii branches at the junction of the proximal third and midthird of the humerus to run posteriorly with the radial nerve to supply the posterior compartment. The brachial artery runs down the arm, lying deep to the bicipital aponeurosis, anterior to the brachialis, and medial to the biceps tendon.
The brachial artery, as well as the profunda, gives off a rich anastomotic network of vessels around the elbow as it moves toward the fossa. Here, it bifurcates into the radial and ulnar arteries. The radial artery crosses deep to the aponeurosis and superficial to the pronator teres and then continues deep to the brachioradialis between the artery and the flexor carpi radialis to the wrist. The radial recurrent is a branch from the radial artery that lies anterior to the lateral humeral condyle to anastomose with the radial collateral branch from the profunda brachii artery.
The ulnar artery passes deep to the pronator teres and lies between the FDS and FDP proximally. Distally, it lies on the FDS between the FDP and FCU. It gives off anterior and posterior recurrent arteries that surround the lateral epicondyle. The common interosseous artery branches from the ulnar artery in the proximal forearm; it immediately branches to form anterior and posterior interosseous arteries. The anterior component passes through the interosseous membrane near the wrist again to join its posterior component.
The musculocutaneous nerve comes from the lateral cord of the brachial plexus. It pierces the coracobrachialis 5-8 cm distal to the tip of the coracoid and branches to supply this muscle, the biceps brachii, and the brachialis. The continuation of this nerve distally serves sensory function as the lateral antebrachial cutaneous nerve.
The radial nerve comes from the posterior cord of the plexus. It enters the posterior compartment through the triangular space between the long head of the triceps and the humerus. It spirals around the humerus from medial to lateral while supplying the triceps muscle. It then pierces the intermuscular septum and emerges between the brachialis and brachioradialis, passing anterior to the lateral epicondyle.
After supplying the anconeus and mobile wad of 3, the radial nerve branches beneath the proximal part of brachioradialis into its two terminal branches, the superficial radial nerve and the posterior interosseous nerve (PIN). The PIN passes under the supinator and eventually lies immediately dorsal to the interosseous membrane. It supplies the remainder of the extensor muscles in the forearm. The superficial radial nerve runs deep to the brachioradialis in the forearm and provides cutaneous sensation to the dorsum of the hand after exiting the forearm between the extensor carpi radialis longus and brachioradialis.
The median nerve arises from the medial and lateral cords of the brachial plexus. It accompanies the brachial artery along the upper extremity. It does not supply any muscles or sensation in the brachium but does provide some fibers to the elbow joint. It passes through the antecubital fossa anterior to the medial epicondyle and deep to the bicipital aponeurosis, lying medial to the brachial artery in most of the population. It exits the fossa medial to the brachial artery and continues into the forearm, splitting the 2 heads of the pronator teres. It runs between the FDS and FDP, supplying all of the superficial flexors of the forearm except the FCU. The anterior interosseous nerve is given off as the median nerve splits the pronator teres. It supplies the deep flexors of the forearm except for the ulnar half of the FDP, specifically FPL and pronator anadratus.
The ulnar nerve is the continuation of the medial cord of the plexus and stays medial to the brachial artery. This courses posterior to the medial epicondyle in its own groove. It provides no motor function in the brachium but does supply some fibers to the elbow joint. It enters the forearm between the 2 heads of the FCU, running distally between the FCU and FDP. It innervates the FCU and the ulnar half of the FDP before entering the hand through the Guyon canal.
Relatively few contraindications exist for fixation of fractures involved with this injury. Patients who sustain severe irreparable vascular compromise may need to undergo emergent amputation to facilitate patient resuscitation. Patients who are critically ill may require a delay in fixation to allow for recovery from the systemic inflammatory response that accompanies these injuries, but open reduction and internal fixation should still be undertaken when appropriate.
Workup
Copyright © www.orthopaedics.win Bone Health All Rights Reserved