

Dislocation of the temporomandibular joint (TMJ; see the image below) is a painful condition that occurs when the mandibular condyle becomes fixed in the anterosuperior aspect of the articular eminence.
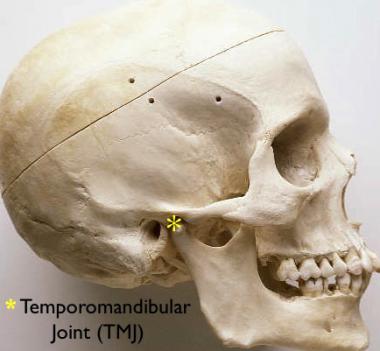 The temporomandibular joint.
The temporomandibular joint.
TMJ dislocation is due to either trauma (force against a partially opened mandible) or, more commonly, excessive opening of the mandible (such as may occur during yawning and dental procedures). Other mechanisms include passionate kissing, eating, yelling, singing, endoscopy, and intubation. Spasm of the masseter, temporalis, and internal pterygoid muscles results in trismus, preventing return of the condyle to the temporal fossa.[1]
More commonly, dislocation occurs bilaterally, resulting in a mandible that is fixed in a symmetrically open position so that only the most posterior teeth may be contacting. Infrequently, unilateral dislocation occurs with resultant deviation of the jaw to the unaffected side.[2]
With dislocation, the mandibular condyles may be palpated anterior to the articular eminence. The diagnosis should be obvious through history and physical examination, and radiographs should not be necessary for confirmation. However, in the setting of trauma, radiographs should be obtained to exclude concomitant fracture.
Patients who have experienced previous dislocation are more prone to recurrence. Additionally, patients with weakness of the joint capsule, anatomic aberration of the joint, or injury to the associated ligaments are at greater risk of dislocation.
NextIndications for reduction of a TMJ dislocation include the following:
Contraindications for reduction of a TMJ dislocation include the following:
The typically intense spasm that occurs with temporomandibular joint (TMJ) dislocation often necessitates the use of substantial analgesia and procedural sedation prior to attempts at reduction. Local anesthesia may be used as an adjunctive measure with 1-2 mL of 1% intra-articular lidocaine but is unlikely to provide adequate pain relief when used alone. (See Procedural Sedation, Pediatric Procedural Sedation, and Local Anesthetic Agents, Infiltrative Administration.)
Equipment employed in reduction of a TMJ dislocation includes the following:
The patient should be seated in an upright position and facing forward, with his or her back and head braced posteriorly. Either a chair with a firm backrest or a low stool placed against a wall may be used. Alternatively, the patient may be positioned with his or her back turned to the practitioner performing the procedure and with the posterior portion of his or her head braced firmly against the practitioner’s body.
Most commonly, reduction of a temporomandibular joint (TMJ) dislocation is performed via the intraoral route.[5] To prevent trauma, the practitioner’s fingers should be gloved with thick gauze taped securely on both thumbs.
Place your thumbs upon the lower molars or on the ridge of the mandible intraorally, posterior to the molars, with your fingers wrapped externally around the mandibles. With the patient positioned so that the mandible is below the level of your elbows, apply firm, slow, and steady pressure in a downward and posterior direction. If bilateral reduction is not possible, reduction may be done one side at a time. (See the images below.)
 Classic reduction technique. The physician places gloved thumbs on the patient's inferior molars bilaterally, as far back as possible. The fingers of the physician are curved beneath the angle and body of the mandible.
Classic reduction technique. The physician places gloved thumbs on the patient's inferior molars bilaterally, as far back as possible. The fingers of the physician are curved beneath the angle and body of the mandible.
 Recumbent approach. The patient is placed recumbent, and the physician stands behind the head of the patient. The physician places his or her thumbs on the inferior molars and applies downward and backward pressure until the jaw pops back into place.
Recumbent approach. The patient is placed recumbent, and the physician stands behind the head of the patient. The physician places his or her thumbs on the inferior molars and applies downward and backward pressure until the jaw pops back into place.
After reduction has been successfully completed, plain radiographs may be obtained to exclude iatrogenic fracture of the mandibular condyles. However, this may not be necessary if reduction resolves the pain.
The patient may wear a soft neck brace, and warm compresses may be placed on the TMJs for comfort. The patient should be instructed to avoid extreme opening of the mouth, such as may occur during yawning, laughing, or dental procedures. Pain relief may be achieved with nonsteroidal anti-inflammatory drugs (NSAIDs), benzodiazepines, or mild opiates.
Patients with chronic dislocations may benefit from the use of a Barton bandage, an elastic bandage that is wrapped around the bottom of the mandible and over the top of the head to prevent excessive jaw opening.
An oral-maxillofacial surgeon or otolaryngologist should be consulted for dislocations that are irreducible, associated with fracture, or immediately recurrent.
Outpatient observation should be arranged to evaluate for possible chronic TMJ pain and ligamentous damage or instability.
Gorchynski et al have described a hands-free "syringe" technique for TMJ reduction that does not require procedural sedation or intravenous analgesia.[6] Of 31 patients with acute nontraumatic TMJ dislocations studied by the investigators at two university centers, 30 (97%) had a successful reduction with this technique, and most of the dislocations (77%) were reduced in less than 1 minute. At 3-day follow-up, there were no recurrent dislocations.
Without adequate sedation, reduction is unlikely to be successful. Agents of choice include midazolam, propofol, and other medications with muscle-relaxant properties.
To prevent injury to the practitioner, the thumbs should be adequately wrapped.
Adequate leverage may be maintained by keeping the mandible below the level of the practitioner's elbows.
Reduction attempts that require excessive force should be aborted because iatrogenic fracture of the mandibular condyles may occur.
Potential complications of reduction of a TMJ dislocation include the following:
Copyright © www.orthopaedics.win Bone Health All Rights Reserved