

The intervertebral disc is the largest avascular structure in the body. It arises from notochordal cells between the cartilaginous endplates, which regress from about 50% of the disc space at birth to about 5% in the adult, with chondrocytes replacing the notochordal cells. Intervertebral discs are located in the spinal column between successive vertebral bodies and are oval in cross section. The height of the discs increases from the peripheral edges to the center, appearing as a biconvex shape that becomes successively larger by about 11% per segment from cephalad to caudal (ie, from the cervical spine to the lumbosacral articulation). A longitudinal ligament attaches to the vertebral bodies and to the intervertebral discs anteriorly and posteriorly; the cartilaginous endplate of each disc attaches to the bony endplate of the vertebral body.
Images of herniated nucleus pulposus are provided below:
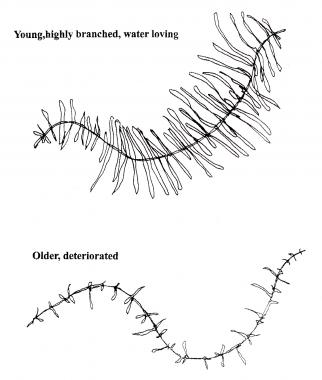 Hyaluronan long chains form a backbone for attracting electronegative or hydrophilic branches, which hydrate the nucleus pulposus and cause a swelling pressure within the annulus to allow it to stabilize the vertebrae and act as a shock absorber. Deterioration within the intervertebral disk results in loss of these water-retaining branches and eventually in the shortening of the chains.
Hyaluronan long chains form a backbone for attracting electronegative or hydrophilic branches, which hydrate the nucleus pulposus and cause a swelling pressure within the annulus to allow it to stabilize the vertebrae and act as a shock absorber. Deterioration within the intervertebral disk results in loss of these water-retaining branches and eventually in the shortening of the chains.
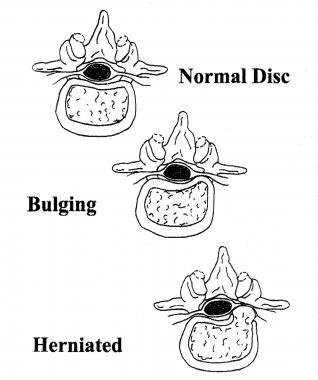 Nuclear material is normally contained within the annulus, but it may cause bulging of the annulus or may herniate through the annulus into the spinal canal. This commonly occurs in a posterolateral location of the intervertebral disk, as depicted.
Nuclear material is normally contained within the annulus, but it may cause bulging of the annulus or may herniate through the annulus into the spinal canal. This commonly occurs in a posterolateral location of the intervertebral disk, as depicted.
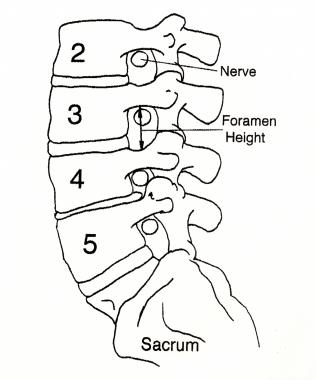 The spinal nerves exit the spinal canal through the foramina at each level. Decreased disk height causes decreased foramen height to the same degree, and the superior articular facet of the caudal vertebral body may become hypertrophic and develop a spur, which then projects toward the nerve root situated just under the pedicle. In this picture, L4-5 has loss of disk height and some facet hypertrophy, thereby encroaching on the room available for the exiting nerve root (L4). A herniated nucleus pulposus within the canal would embarrass the traversing root (L5).
The spinal nerves exit the spinal canal through the foramina at each level. Decreased disk height causes decreased foramen height to the same degree, and the superior articular facet of the caudal vertebral body may become hypertrophic and develop a spur, which then projects toward the nerve root situated just under the pedicle. In this picture, L4-5 has loss of disk height and some facet hypertrophy, thereby encroaching on the room available for the exiting nerve root (L4). A herniated nucleus pulposus within the canal would embarrass the traversing root (L5).
The disc's annular structure is composed of an outer annulus fibrosus, which is a constraining ring that is composed primarily of type 1 collagen. This fibrous ring has alternating layers oriented at 60° from the horizontal to allow isovolumic rotation. That is, just as a shark swimming and turning in the water does not buckle its skin, the intervertebral disc has the ability to rotate or bend without a significant change in volume and, thus, does not affect the hydrostatic pressure of the inner portion of the disc, the nucleus pulposus.
The nucleus pulposus consists predominantly of type II collagen, proteoglycan, and hyaluronan long chains, which have regions with highly hydrophilic, branching side chains. These negatively charged regions have a strong avidity for water molecules and hydrate the nucleus or center of the disc by an osmotic swelling pressure effect. The major proteoglycan constituent is aggrecan, which is connected by link protein to the long hyaluronan. A fibril network, including a number of collagen types along with fibronectin, decorin, and lumican, contains the nucleus pulposus.
The hydraulic effect of the contained, hydrated nucleus within the annulus acts as a shock absorber to cushion the spinal column from forces that are applied to the musculoskeletal system. Each vertebra of the spinal column has an anterior centrum or body. The centra are stacked in a weightbearing column and are supported by the intervertebral discs. A corresponding posterior bony arch encloses and protects the neural elements, and each side of the posterior elements has a facet joint or articulation to allow motion.
The functional segmental unit is the combination of an anterior disc and the 2 posterior facet joints, and it provides protection for the neural elements within the acceptable constraints of clinical stability. The facet joints connect the vertebral bodies on each side of the lamina, forming the posterior arch. These joints are connected at each level by the ligamentum flavum, which is yellow because of the high elastin content and allows significant extensibility and flexibility of the spinal column.
Clinical stability has been defined as the ability of the spine under physiologic load to limit patterns of displacement so as to avoid damage or irritation to the spinal cord or nerve roots and to prevent incapacitating deformity or pain caused by structural changes.[1] Any disruption of the components holding the spine together (ie, ligaments, intervertebral discs, facets) decreases the clinical stability of the spine. When the spine loses enough of these components to prevent it from adequately providing the mechanical function of protection, surgery may be necessary to reestablish stability.
See the list below:
Low back pain (LBP) is ubiquitous, with 60-80% of people having an activity-limiting episode at least transiently in their lifetime. Genetic factors appear to have a dominant role, with LBP starting at an earlier age than previously suspected on the basis of subsequent structural changes; men begin having LBP about a decade earlier than women.[9]
The water-retaining ability of the nucleus pulposus, or the inner portion of the intervertebral disk, declines progressively with age. The decline in the mechanical properties of the nucleus pulposus is associated with the degree of proteoglycan deterioration and the decrease in hydration, which lead to excessive regional peak pressures within the disk. As the hyaluronan long chains shorten and swelling pressure decreases as a result of this deterioration, the mechanical stiffness of the intervertebral disk decreases, which causes the annulus to bulge, with a corresponding loss of disk and foramina height.[10]
The etiology of back pain for a particular individual cannot be determined because of the multiplicity of potential sources. Although periosteal disruption causes pain with fractures, bone itself is devoid of pain receptors (eg, asymptomatic compression fractures commonly are seen in the thoracic spine of elderly individuals with osteoporosis). However, the degenerating intervertebral disk is known to have neurovascular elements at the periphery, including pain fibers. Disk deterioration and loss of disk height may shift the balance of weightbearing to the facet joint; this mechanism has been hypothesized as a cause of LBP through the facet joint capsule, as well as through other tissues attached to and between the posterior bony elements.
When the annulus in animals is incised, a degenerative cascade is initiated that mimics the natural aging process observed in humans, thus providing a model of disk deterioration.[11] As the use of discography has increased for various clinical applications, similar annular tears are seen routinely that are associated with the degeneration of the intervertebral disk, even in patients who are asymptomatic. Annular tears may simply be the result of aging and the degenerative cascade.
Pathology studies of young patients who died as a result of trauma reveal a surprising degree of articular surface damage in the facet joints; magnetic resonance imaging (MRI) routinely reveals disk deterioration in individuals in the second or third decade of life. Injection of chymopapain into the intervertebral disk causes a repeatable and predictable degenerative cascade in the facet joints, illustrating the coupling between the disk and facet joints. Immobilization by facet fusion posteriorly leads to disk deterioration; this avascular structure is solely dependent upon motion to facilitate the diffusion of nutrients into it. Whether the deterioration of the disk or that of the facet comes first has not been determined; however, deterioration is known to occur in both.
Dehydration results from shortening of the hyaluronic chains, deterioration of the state of aggregation, and decreases in the ratio of chondroitin sulfate to keratan sulfate, leading to the disk bulging and disk height loss. The consistency of the nuclear material undergoes a change from a homogeneous material to clumps, which leads to the altered distribution of pressures within the disk and resistance to the flow of nuclear material; the nuclear material thereby becomes mechanically unstable.[12] The clumping of the degenerating nuclear material can be likened to a marble held between 2 books—that is, it is difficult to contain.
These clumps may be lateral to the posterior longitudinal ligament and, therefore, may have the least resistance to herniating through the corner of the intervertebral disk and into the spinal canal or foramen. Surgical removal of the herniated fragments is achieved by grasping them with a pituitary rongeur. This method of surgical removal is not possible with normal, homogeneous material, which is encountered when healthy interverterbral disks are excised anteriorly in patients having surgery because of deformity or trauma. Using the pituitary rongeur technique to perform a microdiscectomy on a herniated fragment necessitates a preexisting state of deterioration; the weakened areas in the annulus provide a path of least resistance for the nuclear material to egress.
Much has been written concerning the process of spinal deterioration or spondylosis, which occurs over a lifetime. Intervertebral disk deterioration leads to decreased stiffness of the disk, as well as diminished stability, resulting in episodic pain that is common and may be temporarily severe. However, continued deterioration ultimately leads to restabilization of the spine by collagenization, which stiffens the disk. Patients in their 50s and 60s customarily have stiffer spines but less pain than patients in their 30s and 40s who are undergoing initiation of the degenerative cascade. Patients who ask if they have to live with this pain "for the rest of their lives" can be reassured to some extent by this natural history. Furthermore, spontaneous recovery from an acute pain episode routinely occurs, so any treatment must be demonstrated as effective by positively altering the expected course without treatment.
In general practice, the overall incidence of herniated nucleus pulposus (HNP) in patients who have new LBP onset is less than 2%. Therefore, most of these patients have deterioration of the intervertebral disk and dysfunction of the functional segmental unit. They will have LBP, and some will have associated leg pain but without sciatica (an intractable, radiating pain, below the knee) or radiculopathy. A disk fragment that is no longer contained within the annulus but is displaced into the spinal canal has decreased hydration and deteriorated proteoglycan that can be expected to undergo further deterioration and consequent annular desiccation, essentially like a grape being transformed into a raisin.
Spontaneous resolution of sciatica may result from shrinkage of a herniated fragment, aided by macrophages and the evoked inflammatory reaction, but practitioners too often attribute this clinical improvement to their favorite treatments. Intractable symptoms of sciatica from intervertebral disk displacements may benefit dramatically from surgical intervention. Within 20 years of Mixter and Barr's 1934 report, Friedenberg compared operative treatment with nonoperative treatment.[13, 14] Nonoperative treatment yielded 3 groups of results: pain free, occasional residual pain, and disabling pain. Proportions of these groups remained similar after 5 years. Friedenberg concluded that even recurrent severe episodes may resolve without surgery; the problem was and remains patient selection.
Weber presented a randomized, controlled study (marred by dropouts in the surgery control group because of severe pain) and concluded that patient results were the same whether treated operatively or conservatively, except that those who were treated operatively had better results at 1 year.[15] The Spine Patient Outcomes Research Trial (SPORT) observational cohort is similarly limited in its conclusions by crossovers: 50% of the surgery arm had surgery within 3 months and 30% of the nonsurgical group had surgery, but at long-term follow-up, both groups again were not statistically different.[16]
Nuclear material that is displaced into the spinal canal is associated with a significant inflammatory response, as has been demonstrated in animal studies. Disk injury results in an increase in the proinflammatory molecules interleukin-1 (IL-1), IL-8, and tumor necrosis factor (TNF) alpha. Macrophages respond to this displaced foreign material and seek to clear the spinal canal. Subsequently, a significant scar is produced, even without surgery, and substance P, which is associated with pain, is detected. Acute neural compression is responsible for dysfunction; compression of a motor nerve results in weakness, and compression of a sensory nerve results in numbness. Radicular pain is caused by inflammation of the nerve, which explains the lack of correlation between the actual size of an intervertebral disk herniation or even the consequent degree of neural compression and the associated clinical symptoms.[17]
Furthermore, intervetebral disk degeneration may result in radial tears and leakage of the nuclear material, which leads to neural toxicity. The subsequent inflammatory response often results in neural irritation causing radiating pain without numbness, weakness, or loss of reflex, even when neural compression is absent.
Several factors seem to influence the occurrence of herniated nucleus pulposus. Smoking is a risk factor in the epidemiology of lumbar disk herniations and has been documented to decrease the oxygen tension in the avascular disk dramatically, presumably by vasoconstrictive and rheologic effects on blood. Lumbar disk herniation may result from chronic coughing and other stresses on the disk. For example, sitting without lumbar support causes an increase in disk pressures, and driving is also a risk factor because of the resonant coupling of 5-Hz vibrations from the road to the spine. People who drive signifcant amounts have increased spinal problems; truck drivers have the additional risk of spinal problems from lifting during loading and unloading, which, unfortunately, is done after prolonged driving.
Studies have shown that peak stresses within a deteriorated intervertebral disk exceed those from average loads on a normal disk, which is consistent with a pain mechanism. Further repetitive stress at physiologic levels did not produce a herniation after prolonged testing, contradicting the concept of injury accumulation with customary work activities. However, after a simulated injury to the annulus (cutting), a lower mechanical stress did result in disk herniation, consistent with intervertebral disk degeneration and with clinical experience on discography.
The presumed traumatic cause of disk herniations has been questioned scientifically in the literature, particularly with the increased availability of genetic information.[18, 19]
The pathologic state of a weakened annulus is a necessary condition for herniation to occur. Many cases involve trivial trauma even in the presence of repetitive stress. An annular tear or weak spot has not been demonstrated to result from repetitive normal stress from customary activities or from physically stressful activities.
Mixter and Barr first recognized that the cartilaginous masses in the spinal canal of their patients were not tumors or chondromas.[13] They proposed that herniation of the nucleus pulposus and displacement of nuclear material caused neural irritation, inflammation, and pain. They showed that excising a disk fragment was effective, but their recommendation to perform this procedure with a fusion was necessitated by relatively aggressive laminectomy. This procedure has been replaced by techniques that are less invasive, such as microdiscectomy.
Obtaining pertinent patient historical information should begin with an analysis of the chief complaint. Does the patient's complaint concern dominant leg pain, dominant back pain, or a mixture of significant problems with both? Next, is the onset acute, subacute, or chronic? Under what circumstances does onset occur? What is the patient's prior history, particularly regarding similar symptoms or treatment response?
Identify risk factors, obtain a pertinent medical history, and specifically exclude red flags, such as nonmechanical pain, which causes pain at night without activities because pressure in the pelvic veins may be increased upon reclining. Nonmechanical pain may be indicative of a tumor or infection. A progressive neurologic deficit or cauda equina syndrome is considered a surgical emergency because irreversible consequences may result if these are left untreated.
Obtaining a thorough history of activity intolerance requires some time and attention to the details of specific examples and the positions or actions that cause problems. Also, it is helpful to determine which activities the patient is unable or less able to perform and which activities exacerbate or moderate the pain. An assessment of the physical demands of the patient's occupation and daily activities provides the perspective for the described activity intolerance. A pain drawing can be very helpful in assessing the pattern of pain, such as a dermatomal distribution, or in assessing the organicity of the complaints.
Physical examination classically involves range-of-motion (ROM) testing of the lumbar and cervical spine, but these findings may be more reflective of aging or deterioration in the intervertebral disks and joints than any quantifiable assessment of impairment. The remainder of the examination is essentially a neurologic assessment of weakness, dermatomal numbness, reflex change, and, most important, sciatic or femoral nerve root tension in the lumbar spine.
Numerous examination maneuvers (eg, Lasegue classic test, Lasegue rebound sign, Lasegue differential sign, Braggard sign, flip sign, Deyerle sign, Mendel-Bechterew sign, well leg test or Fajersztajn sign, both-legs or Milgram test) are available but cloud the issue, because the sciatic nerve root tension or straight-leg raising test is the basis for nearly all of them. They are essentially modifications for subtle differences, but the provocation of radiating pain down the leg is of a neural compressive lesion and compression of the sciatic nerve root, if it goes below the knee. Furthermore, the provocation of radiating pain down the leg is the most sensitive test for a lumbar disk herniation.
For a higher lumbar lesion, reverse straight-leg raising or hip extension that stretches the femoral nerve is analogous to a straight-leg raising test. The Spurling test in the cervical spine is used to detect foraminal stenosis (Kemp's test is used in the lumbar region) rather than specifically for intervertebral disk herniation or nerve root tension. Careful hip, rectal, and genitourinary examinations help exclude complications of those organ systems in the diagnosis of higher lumbar lesions.
After obtaining plain radiographs, further imaging studies (eg, MRI, computed tomography [CT] scanning, CT myelography) may be indicated to assess degenerative disk disease, loss of disk height, and facet deterioration, such as sclerosis or hypertrophy. MRI clearly provides the most information, perhaps too much, as it has a 25% false-positive rate (asymptomatic herniated nucleus pulposus [HNP]). An HNP that is noted on imaging studies must be correlated with objective examination findings; otherwise, it must be presumed to be an asymptomatic HNP if there is no correlation between the imaging findings and pain or clinical symptoms. Therefore, imaging studies should perhaps be reserved for cases in which positive physical findings have been documented.
Other causes of significant back pain in the absence of neurologic findings should be considered. Sciatic nerve irritation may result from sacroiliac dysfunction or degenerative joint disease caused by the proximity of the sciatic notch to the sacroiliac joint or peripheral entrapment, including piriformis syndrome. Careful examination with an adequate differential for the diagnosis may prevent prolonged ineffective empirical care for presumed lumbar disk disease.
The facet syndrome has been controversial, but neurophysiologic studies have shown discharges from the capsule consistent with pain, as well as inflammation and degenerative joint disease.[20] However, large numbers of patients have reported significant relief after facet joint injections for nonspecific LBP; as a result, the facet syndrome has become more widely accepted. Clinically, patients usually have pain only to the knee, not below, as would be expected from an HNP.
Spontaneous improvement of low back discomfort has allowed ineffective treatments to perpetuate, because benefits have been ascribed to them when they are prescribed while the patient is still symptomatic but otherwise improving. Hippocrates expected improvement in sciatica in 40 days, and the customary and contemporary guideline is 6 weeks. An often-quoted study suggests near-resolution improvement of 90% of patients within 6 weeks, but this study has been faulted because the criterion for patient recovery was failure to return to the observing physician.[21] The prevalence of back problems is consistent with the failure of a subgroup of patients to improve and to have periodic recurrent episodes of disability.
Analysis of the effectiveness of treatments and attempts to restrict treatment to those modalities that have demonstrated efficacy are evidence-based medical practice. Bedrest has a long history of use but has not been shown to be effective beyond the initial 1 or 2 days; after this period, bedrest is counterproductive. All conservative treatments are essentially efforts to reduce inflammation; therefore, only a very short period of rest is appropriate, anti-inflammatories are of some benefit (because the pain is from inflammation of the nerve), and warm, moist heat or modalities may be helpful. TNF α ηασ βεεν εξπεριμενταλλψ σηοων το decrease in preclinical models.[22] Activities should be resumed as early as tolerated. Exercises and physical therapy mobilize muscles and joints to facilitate the removal of edema and promote recovery. Muscle relaxants mayoffersymptomatic relief of the acute muscle spasms but only in the early stages; however, all are central acting, there is no direct relaxation of skeletal muscle, and they are also sedating.
For back pain without radiculopathy, chiropractic care has high patient satisfaction when performed within the first 6 weeks, and it has been shown to have good efficacy acutely from an evidence-based standpoint.[23] Injections (eg, epidural) may be particularly helpful in patients with radiculopathy by providing symptom relief, which allows the patient to increase activities and helps facilitate rehabilitation.[24, 25] Any nuclear material that is herniated may shrink as the proteoglycan deteriorates, loses its water-retaining ability, and turns from a grapelike object to a raisinlike object.
Arbitrary time schedules for improvement are inappropriate in any patient who continues to improve and whose function is relatively maintained. Traction in the acute setting may help muscle spasms, but it does not reduce the HNP and has no good evidence of efficacy. The use of traction does not justify hospital admission, as it is not cost-effective and can be administered on an outpatient basis.
Long-term use of physical therapy modalities is no more effective than hot showers or hot packs are at home. A transcutaneous electrical nerve stimulation (TENS) unit may be subjectively helpful in some patients with chronic conditions. Encourage patients to essentially compensate for intervertebral disk incompetence, as possible, by muscular stabilization, and to maintain flexibility by initiating life-long exercise regimens, including aerobic conditioning, particularly swimming, which allows gravity relief.
Assess the body mechanics of every patient who is disabled from work. Educate all patients about body mechanics, and discuss the risk factors for faulty body mechanics, so that applications can be incorporated into individual work settings, including appropriate seating (eg, lumbar support). The lumbar facet joints are oriented relatively vertically, thus allowing forward flexion, but the joints impact each other when a person bends and then rotates. Repetitive bending and twisting have been noted to be epidemiologic problems in workers, and may be associated with chronic pain and disability.[26] Attention to lifting techniques and ergonomic modification at workstations may be very appropriate.
The classic presentation of an herniated nucleus pulposus includes the complaint of sciatica, with associated objective neurologic findings of weakness, reflex change, and dermatomal numbness. Various surgical procedures have been reported and share the common goal of decompressing the neural elements to relieve the leg pain. These procedures are most appropriate for patients with minimal or tolerable back pain, with an essentially intact and clinically stable disk. However, the hope of permanently relieving the back pain is a fantasy, a false hope.
The most common procedure for a herniated or ruptured intervertebral disk is a microdiscectomy, in which a small incision is made, aided by an operating microscope, and a hemilaminotomy is performed to remove the disk fragment that is impinging on the nerves.
Many patients who undergo microdiscectomy can be discharged with minimal soreness and complete relief of leg pain after an overnight admission and observation. Same-day procedures are in the process of cautious development; patients with dominant back pain have a different problem, even if HNP is present, and would require stabilization by fusion if unresponsive to well-managed appropriate therapy or arthroplasty (if there is an isolated level with good facet joints).
Minimally invasive techniques have not replaced this standard microdiscectomy procedure but can be summarized in 2 categories: central decompression of the disk and directed fragmentectomy. Outpatient treatment has been reported.[27]
Central decompression of the disk can be performed chemically or enzymatically with chymopapain, by laser or plasma (ionized gas) ablation and vaporization, or mechanically by aspiration and suction with a shaver such as the nucleotome or percutaneous lateral decompression (arthroscopic microdiscectomy).
The Food and Drug Administration (FDA) initially released and then withheld chymopapain for injection into lumbar disks because of adverse allergic reactions in patients; skin tests subsequently were used to determine sensitivity. However, the procedure continued to induce severe muscle spasms that could be far worse than those of an open operation and thus required hospitalization and bedrest for up to 50% of patients.[28] This morbidity must be considered a contradiction to the assertion by proponents that the enzyme is limited to the disk in the chemical digestion of the nucleus pulposus, because the muscles are severely affected, which would not be expected if the enzyme were contained. In addition, severe scarring in the spinal canal is noted routinely after this procedure.
The nucleotome and laser central decompressions have been shown only to equal placebo in effectiveness, and their use has declined. Superiority has not been demonstrated; patient selection is crucial, with a steep learning curve.[29]
Further development of alternatives, such as nucleoplasty, and efforts to reduce disk pressure remain under study. The incidence of recurent herniation is small but may be irreducible. Efforts to seal the annulus are under investigation.
Directed fragmentectomy is similar to an open microdiscectomy and has demonstrated greater effectiveness than placebo. This procedure uses an arthroscopic approach and a probe that directs a flexible pituitary rongeur from the center of the intervertebral disk toward the posterior annulus. Endoscopic techniques to perform a directed fragmentectomy and to minimize disruption of normal structures continue in development, but superiority has not been demonstrated despite this minimally invasive approach.
Concerning the cervical spine, HNP customarily is treated anteriorly, because the pathology is anterior and manipulation of the cervical cord is not tolerated by the patient. The posterior approach is reserved for disk herniation that is confined to the foramen and for foraminal stenosis. An alternative to the anterior cervical spine approach is minimal disk excision; clinical stability following this procedure is dependent upon the residual disk, which is also true in cases where there is lumbar spine involvement with back pain. Removal of neural compression dramatically relieves radiculopathy; however, residual axial neck pain may result in significant impairment.
Anterior cervical interbody fusion is another intervention. Proponents of discectomy alone assert equivalent results, but the adequacy of follow-up in those case reports is a significant concern. Patients with more severe disk degeneration, particularly myelopathy, would more uniformly undergo fusion. Anterior instrumentation is being used more commonly, and interbody cages are under consideration as a means of attaining more rapid rehabilitation and more consistent results. Multilevel disc replacement has been suggested as at least similar to fusion.[30]
The diagnosis of an internal disk derangement is controversial. The classic patient presents with back pain without imaging abnormalities except for varying degrees of the black disk, which is the converse of the asymptomatic patient with an intervertebral disk herniation. Patients without a disk herniation have a favorable course and long-term outcome with conservative treatment or surgery. However, some patients with prolonged limitations and limited job skills benefit from surgical intervention for segmental instability or clinical instability as we earlier discussed. A positive discogram properly done and carefully interpreted in context may raise the expectation of success for surgical treatment in this patient population. The greatest controversy is over the effectiveness of fusion surgery. Unfortunately, there is no clear objective criterion; clinical judgment is mandatory and is not perfect; clearly, good patients do well, and patient selection is paramount.
Patients with "broad-based" intervertebral disk herniations generally have a deterioration of the disk or a failure of clinical stability with associated back pain, rather than isolated sciatica. These patients are not appropriate candidates for microdiscectomy alone. Lumbar fusion is being used increasingly in these cases, and arthroplasty is also being considered; however, this treatment remains controversial because it is, again, based inevitably on subjective patient pain and clinical judgment without objective determination. Many reports in the literature have described specific cytokines elevated, but not comprehensively; endplate changes are observed but no clear correlation identified to this point. Various nuclear replacements that reduce postoperative loss of disc height restoring compressive loading are being studied.[31]
With a discectomy, patients with dominant leg pain have excellent results, with 85-90% returning to full function. However, up to 15% of patients have continued back pain that may limit their return to full function, despite the absence of radiculopathy. Patients who undergo surgery do not necessarily show better results than patients who defer surgery.[32] The remaining concern of recurrent herniation is small, although is is correlated with obesity.[33] Efforts to minimize this complication have included annulus repair[34] and injecting hemostatic materials or bioactive molecules. Etanercept was shown in a small study to be of no benefit for sciatica, although the addition of butorphanol with corticosteroid was helpful with an epidural injection.[35]
Intervertebral disk degeneration that causes clumping of the nuclear material and relative mechanical instability is the necessary preceding condition for HNP. However, it is impossible to tell which patients will do well after microdiscectomy for a herniation and which will have continued problems, of varying severity, from the disk degeneration. Studies have shown that degenerated discs have different growth factors and other molecules; thus, even introducing mesenchymal stem cells requires significant further research and development.[36] Significant deterioration and accompanying LBP increasingly are being treated with stabilization, via either an anterior lumbar interbody fusion (ALIF) or a posterior lumbar interbody fusion (PLIF) in association with posterior decompression (when necessary) and instrumentation. Results are not yet available, as techniques are still evolving, but experience is accumulating.
Copyright © www.orthopaedics.win Bone Health All Rights Reserved