

Dislocation of the radial head occurs most frequently in men who are subject to high-force injury.[1]
In children, the radial head is much more commonly subluxed than it is dislocated. (See Radial Head Subluxation Joint Reduction.)
The radial head can be congenitally dislocated in isolation or in conjunction with other congenital abnormalities such as those in Steel syndrome and achondroplasia.[2, 3, 4, 5] Radial head dislocations may be seen in association with the rare isolated interosseous membrane injury of the forearm.[6] Isolated radial head dislocations are exceedingly rare.[7] Radial head dislocations are usually complicated by complete elbow dislocations or fractures, as in the Monteggia complex. Radial head dislocations have also been rarely seen with associated humeral condyle fracture.[8]
Monteggia described the combination of radial head dislocation and proximal ulnar fracture in 1814. More than a century later, Bado[9, 10] further classified the Monteggia injury into four types on the basis of the angulation of the fracture and the direction of dislocation (see Table 1 below).[11] The Bado classification is useful descriptively but not prognostically.
Table 1. Bado Classification of Monteggia Injuries (Open Table in a new window)
Classification Incidence Description Type I 60% Fracture of the proximal or middle third of the ulna with anterior angulation and anterior dislocation of the radial head Type II 15% Fracture of the proximal or middle third of the ulna with posterior angulation and posterior dislocation of the radial head Type III 20% Fracture of the ulnar metaphysis distal to the coronoid process with lateral dislocation of the radial head Type IV 5% Fracture of the proximal or middle third of the ulna and fracture of the proximal third of the radius with anterior dislocation of the radial headRadial head dislocation is often associated with significant trauma (eg, motor vehicle accidents, pedestrian–motor vehicle accidents, significant falls). The proposed mechanism is force directed onto an outstretched, pronated arm.[12] Other mechanisms of injury, such as hyperextension of the elbow with the forearm in mid prone position, have been reported.[7]
A person with a radial head dislocation typically holds his or her elbow flexed at 90º and resists passive and active range of motion at the elbow, including pronation and supination. The elbow is often swollen and diffusely tender with increased point tenderness over the radial head (see the image below). In the case of Monteggia fracture, crepitus may be present over the proximal ulna. The radial head may be palpable in an anterolateral or posterolateral location, and the forearm may appear shortened and angulated.
 Swollen elbow from a radial head dislocation.
Swollen elbow from a radial head dislocation.
Radial head dislocations are easily missed on radiographs and therefore require a high index of suspicion.[13, 14, 15] Undiagnosed chronic radial dislocations lead to poor outcome, limited function, and chronic pain.[16] The therapeutic goals are as follows[17] :
In patients with suspected injury, standard anteroposterior, lateral, and oblique radiographs should be taken of the elbow and forearm (see the images below). (See Elbow, Fractures and Dislocations - Adult.)
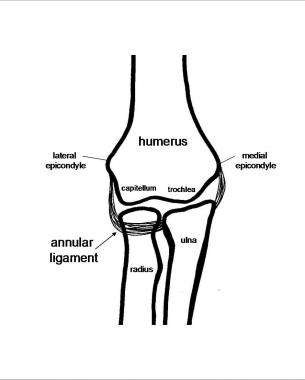 Elbow Anatomy
Elbow Anatomy
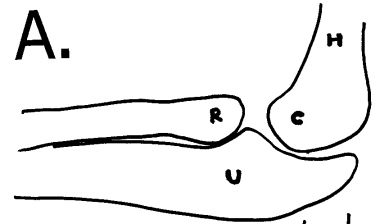 Landmarks on lateral elbow radiograph: radial head (R), ulna (U), capitellum (C), and humerus (H).
Landmarks on lateral elbow radiograph: radial head (R), ulna (U), capitellum (C), and humerus (H).
The radiocapitellar line can be used to evaluate for subluxations and dislocations of the radial head.[18] This line, drawn through the long axis/body of the radius, normally bisects the capitellum in any degree of flexion or extension (see the image below).[19] Deviation of this line suggests capitellar or radial dislocation.
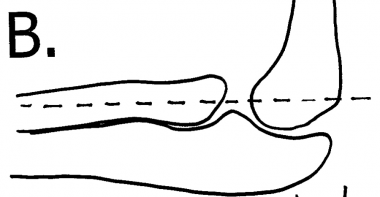 Normal radiocapitellar line drawn from radius through the mid capitellum.
Normal radiocapitellar line drawn from radius through the mid capitellum.
Be sure to carefully evaluate the ulna for any fracture or plastic bowing deformity to suggest a Monteggia complex.[20] In a Monteggia fracture, the apex of the ulnar fracture points in the direction of the radial head dislocation (see the image below).
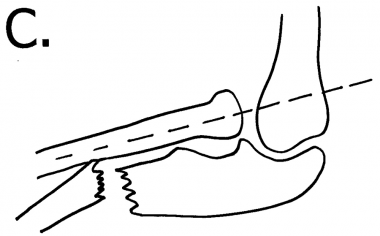 Abnormal radiocapitellar line due to dislocation of radial head. Line does not bisect capitellum. The apex of the ulnar fracture points in the direction of the radial head dislocation (anteriorly, in this case).
Abnormal radiocapitellar line due to dislocation of radial head. Line does not bisect capitellum. The apex of the ulnar fracture points in the direction of the radial head dislocation (anteriorly, in this case).
The management of a radial head dislocation is dictated by the presence or absence of an associated fracture. If an associated fracture is present, the forearm is not considered stable; in such a case, bedside reduction of a radial head dislocation is not appropriate. Although operative repair is recommended in adults, a conservative approach may be considered in children with Monteggia injuries.[21, 22]
Open and complex radial head dislocations as well as Monteggia fractures in adults necessitate consultation with an orthopedic or hand surgeon.[23] Such injuries are usually reduced with fixation in the operating room.[24, 25, 26]
NextSplinting supplies are needed for the period following reduction. If procedural sedation is used, the standard monitoring equipment is necessary.
Anesthesia
Reduction is optimally performed on a relaxed and comfortable patient by using one of the following methods:
Positioning
For most reduction techniques, the patient may sit upright or lie supine. Bado suggested that reduction be performed in the opposite direction of the external force at the time of injury and that the forearm be immobilized in this position.[10]
Most injuries occur in a pronated position; therefore, after reduction, splint the forearm in the supinated position with 90° elbow flexion.
Assess and document the neurologic and vascular status of the arm. Further evaluate the arm on the basis of the type of injury (see below).
Monteggia injuries were once treated nonoperatively in adults. However, surgical treatment of these injuries results in decreased pain, less restricted motion, decreased valgus, and less late neuropathy.[27, 28, 29, 30, 31] Once the ulna is fixed, often by means of operative compression plating,[32, 33] the radial head often self-reduces. If orthopedic or surgical care is not immediately available, the practitioner who provides initial treatment may splint the fracture and perform reduction as instructed below, with prompt referral to a specialist.
Although operative repair is recommended in adults, a conservative approach is often used in children with Monteggia injuries.[21, 22, 34] Children may be treated by means of closed reduction of both bones and immobilization in a long arm cast.[35] The key to reduction in children is to obtain normal length and alignment of the ulna, after which the radial head typically falls into place. When necessary, open reduction with internal fixation (ORIF) is performed.[36]
Some advocate primary operative care in complete ulnar fractures because of the shortening and angulation that may occur without fixation. In general, surgical repair of ulnar fractures in children may involve relatively smaller plates and screws than those used in adults because of rapid osseous repair. In transverse and short oblique fractures, an intramedullary wire may be used.
Surgical pearls
Be wary of other serious associated injuries, especially to the head and chest.
Carefully evaluate the bones and joints above and below the injury.
Always assess and document the neurologic and vascular status of the arm before and after reduction.
Before discharging a patient with a forearm or elbow injury, always use the radiocapitellar line to check any misalignment of the radial head.[37] This is especially important in the case of an ulnar fracture.
Delayed treatment
Many radial head dislocations are missed on initial presentation and may be diagnosed years later.[38] Previously undiagnosed radial head dislocations are fixed operatively in adults and are usually fixed operatively in children.[39, 40] . After 3 years of dislocation, deformities develop in the radial head (dome shape deformity) and radial notch of the ulna.[41]
A retrospective review showed a high success rate with surgical management of chronic posttraumatic anterior dislocation of the radial head in children.[42]
The triceps tendon can be used to reconstruct the annular ligament through techniques described by Bell Tawse,[43, 44] Lloyd-Roberts, and Bucknill.[45] DeBoeck described a procedure without annular ligament reconstruction.[46]
At times, the nonreducible radial head may have to be excised.[47] Seel, Peterson, and Papandera have also described alternative reduction techniques.
Closed reduction
Nonsurgical treatment may be considered in children. The key to success is proper reduction of the ulnar fracture. Reestablish the proper length of the ulna, and correct any angulation. Once the ulna is reduced, the radial head is easily replaced. With the elbow flexed 115° to relax the biceps, provide longitudinal traction and fully supinate the arm while applying posterior manual pressure to the proximal radius anteriorly. Splint the arm in 90° flexion and supination, using three-point molding to counteract the forearm musculature.
Repeat radiographs in 1 week to assess continued proper reduction. A long-arm cast may be used for 3 weeks, followed by 3 weeks in a short-arm cast.
Open reduction
Open reduction is indicated in cases of failure to maintain ulnar or radial anatomic position. Ulnar osteotomy with elongation and reduction of the angulation is performed along with open reduction of the radial head.[48]
Closed reduction
Reduction is accomplished with longitudinal traction with the elbow extended because the ulna is most stable with the arm extended. The radial head is reduced with pressure directed anteriorly onto the radial head. Once reduction has been accomplished, three-point cast molding is placed with the elbow in extension and pronation (70° of flexion).
This metaphyseal fracture heals quickly and the cast can usually be removed in 3 weeks. However, immobilization must continue until union of the ulna occurs, which may take as long as 10 weeks in older patients. Flexion may return slowly.
Open reduction
Operative indications are the same as those for type I Monteggia injuries.
Closed reduction
The incidence of posterior interosseous nerve injury is high with this lesion[49] ; however, such injury typically resolves spontaneously and rapidly. Reduction is accomplished by hyperextension and stabilization of the olecranon followed by a valgus force to the olecranon. This force corrects the greenstick fracture, and the radial head often spontaneously reduces. If necessary, direct medial pressure to the radial head facilitates reduction.
Controversy exists concerning the best type of immobilization for a type III injury. Some advocate splinting, as in type I Monteggia injuries (115° of flexion), and some recommend immobilization in a long arm cast in extension with valgus stress applied to the ulna.[50] The cast should be maintained for 4-6 weeks.
Open reduction
This type of injury is most commonly irreducible because of annular ligament interposition.
Closed reduction
Nonoperative methods for this unstable fracture are difficult and often unsuccessful.
Open reduction
Unlike the other three types of Monteggia injury, type IV lesions usually necessitate initial surgical stabilization of the radius and ulna fractures. The elbow is immobilized in supination and hyperflexion (115°) in a long arm cast for 3 weeks. A short arm cast is applied for an additional 3–4 weeks.
Anterior
Supinate the arm, and flex the elbow to 115° to relax the biceps. An assistant holds the humerus distally for stabilization while the practitioner applies distal traction to the wrist and direct posterior pressure to the radial head.[51, 52, 53, 54, 55, 56] (See the video below.)
Technique for reduction of an anterior radial head dislocation.Posterior
The arm is held supinated in extension at the patient’s side, and the humerus is stabilized distally.[57] With care taken not to hyperextend the arm, distal traction is placed at the wrist, and anterior pressure is applied to the radial head. (See the video below.)
Technique for reduction of posterior radial head dislocation.Lateral
As with the technique used in a posterior reduction, provide stabilization to the distal humerus and place distal traction at the wrist while applying medial pressure to the radial head. (See the video below.)
Technique for reduction of lateral radial head dislocation.Failure to reduce
In some instances, the elbow is not reducible with closed reduction techniques, and operative repair is necessary. Possible reasons for this include delayed treatment,[58] presence of interposed tissues that impede reduction, and an extremely unstable elbow. In rare cases, osteosynthesis or resection of the radial head may be necessary.
Chronic dislocation of the radial head is rare and often goes undiagnosed. These dislocations may be of either congenital or traumatic origin.[59] Although they are initially asymptomatic, arthritic changes may restrict movement as time goes on.[60] Long-term dislocations often result in valgus deformity of the elbow, which may subsequently result in ulnar and interosseous nerve disturbance.[59] Furthermore, when the radial head is left dislocated for an extended period, anatomic changes begin to occur to the radial head and radial notch of the ulna.[41] Treatment of chronic radial head dislocation is controversial, ranging from neglect to ORIF.
Closed reduction is based on the direction of dislocation as outlined above.
Surgical intervention is recommended to restore function, relieve pain, and improve cosmetic appearance.[59] Open repair of the ulna is made if necessary. For the chronically dislocated radius, two surgical options are available: resect or preserve the radial head. Advocates of radial head–sparing reconstructions have touted fewer complications and substantial pain relief; however, improvement of range of motion (ROM) is limited, and additional surgery is needed 25% of the time.[59, 61] Radial head–sparing techniques include reconstruction and reattachment of the annular ligament and/or osteotomy of the radius or ulna.[59, 62]
Once reduction is complete, reassess and document the neurologic and vascular status of the arm. Evaluate the elbow in its full ROM (varus, valgus, pronation, supination) and check for soft tissue, bony blocks, or other instability. Apply a posterior splint in 90° flexion, and supinate for isolated dislocations.
Obtain postreduction radiographs and reevaluate the radiocapitellar line. If reduction is performed in the operating room, the stability of the radial head may be checked under fluoroscopy. Patients are generally admitted for 24 hours to observe for possible complications such as compartment syndrome.
The ROM exercises can be initiated when pain and swelling permit. Frequent radiographs should be taken to confirm that the elbow remains reduced during early rehabilitation. In isolated radial head dislocations, range of motion is instituted within a few days and the splint is generally discontinued after 1-2 weeks if the elbow is deemed stable. Unstable elbows require longer immobilization.
After such an injury, a loss of 5-10° of extension in comparison with the contralateral elbow can be expected; however, uncomplicated radial head dislocations have a favorable prognosis.[63]
Follow-up with an orthopedist is mandatory.
Complications include the following:
Copyright © www.orthopaedics.win Bone Health All Rights Reserved