

Carpal tunnel syndrome (CTS) is a common mononeuropathy due to entrapment of the median nerve in the carpal tunnel. Symptoms include hand paresthesia, numbness, and pain in the median nerve distribution of the hand. Conservative treatment options, in addition to carpal tunnel steroid injection, include rest, splinting, oral steroids, ultrasound, yoga, physical therapy, and ergonomic modification.[1] Surgical intervention is reserved for severe symptoms.
Clinical testing for carpal tunnel syndrome includes the Tinel test, which is performed by lightly tapping the median nerve eliciting paresthesia in the nerve distribution of the hand. Additional testing includes the Phalen test, which increases pressure in the carpal tunnel by forced wrist flexion for several minutes.
Carpal tunnel steroid injection has been shown to reduce short-term symptoms prior to definitive surgical intervention. Local steroid injection and surgical decompression both are effective treatments at 2-year follow-up, with surgical intervention having some additional benefit.[2]
Electrodiagnositc studies such as nerve conduction studies and electromyography can be used to determine median nerve compression severity.
The wrist is a complex joint consisting of the distal portion of the radius and ulna articulating with eight carpal bones which in turn articulate with the proximal aspects of five metacarpal bones. Together, these bones are responsible for flexing and extending, pronating and supinating as well as ulnar and radial deviation.
The carpal tunnel is defined ventrally by the flexor retinaculum, attached radially to the scaphoid and trapezium, and the pisiform and hamate on the ulnar side. The carpal bones define the dorsal border of the carpal tunnel. The carpal tunnel contains four tendons of the flexor digitorum profundus, four tendons of the flexor digitorum superficialis as well as the flexor pollicis longus tendon. Just deep to the flexor retinaculum is where the median nerve traverses the carpal tunnel. This branch of the median nerve supplies the sensory innervation of the first three digits and the radial half of the fourth digit.
For more information about the relevant anatomy, see Wrist Joint Anatomy.
NextSee the list below:
See the list below:
See the list below:
See the list below:
Have the patient seated or in supine position with affected wrist supinated resting on the small rolled towel allowing for wrist dorsiflexion.
Identify the flexor carpi radialis (lateral) and palmaris longus tendons (medial). Prep the skin using the antiseptic solution.
Using the 25 ga needle make a skin wheel with 1% lidocaine just medial to the palmaris longus tendon and approximately 1 centimeter proximal to the wrist crease.
In a separate syringe draw up the steroid and enter the skin at the skin wheel just medial to the palmaris longus tendon using blunt tip 25 ga needle. Direct the needle toward the third digit at a 30 degree angle. Advance the needle approximately 1.5 -2 cm. Aspirate to verify that the needle is not intravascular and inject the steroid with little or no resistance.
Remove the needle and place the wrist in a gravity-dependent position advising the patient to move the fingers for several minutes to facilitate even distribution of the solution.
The landmark procedure is shown in the video below.
Steroid injection, carpal tunnel.Several approaches to ultrasound guided carpal tunnel injections have been described.
Out of plane approach/Short axis view
Using a high frequency ultrasound transducer held transverse across the wrist, the median nerve is identified under the flexor retinaculum. The needle is advanced out of plane, proximal to the ultrasound transducer and directed toward the third digit. Once under the flexor retinaculum the steroid solution is injected with low resistance to surround the median nerve.
In-plane approach/Short axis view
By using a high frequency ultrasound probe the wrist is imaged by placing the probe transverse across dorsiflexed wrist. The median nerve and ulnar artery is identified. At the level of the distal wrist crease, the needle is passed into the skin superficial to the ulnar artery, penetrating the flexor retinaculum. The needle is advanced toward the median nerve. The steroid solution is injected just under the flexor retinaculum then retracted and redirected deeper to the ulnar side of the median nerve. This allows the median nerve to be completely surrounded with the steroid solution.[3]
 Short-Axis View Ultrasound Probe Placement
Short-Axis View Ultrasound Probe Placement
 In-Plane Approach with block needle
In-Plane Approach with block needle
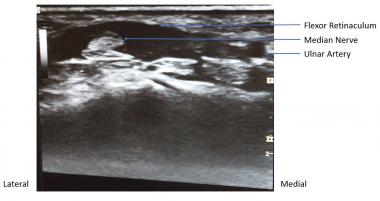 Short-Axis View
Short-Axis View
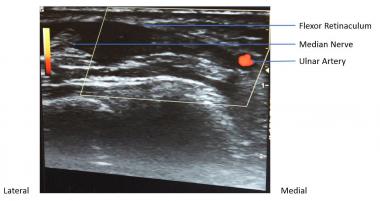 Short-Axis View with Dopplar
Short-Axis View with Dopplar
Sudden pain or paresthesia during the procedure can be indicative of improper needle placement. The needle should be retracted and redirected more medial.
Some patients lack a palmaris longus tendon in which case the insertion point of the needle should be halfway between the radial and ulnar aspects of the wrist and about 1cm proximal to the wrist crease. The needle should be advanced toward the ring finger.
Complications may include the following:
Copyright © www.orthopaedics.win Bone Health All Rights Reserved