

Arthrocentesis involves both the puncture of a joint and the aspiration of its synovial fluid. It is typically used to make an accurate diagnosis of a painful, warm, swollen joint. Removal of excess fluid can be therapeutic. Analysis of the removed fluid helps to decipher its etiology.[1]
The most emergent diagnosis of consideration, a septic joint, occurs less frequently in the elbow than in larger joints (5-10%), with the exception of cases in which Neisseria gonorrhoeae is the pathogen.[2, 3] See Aspiration Techniques and Indications for Surgery, Septic Arthritis for more information.
NextBefore the procedure, periarticular processes such as bursitis, tendonitis, contusions, and cellulitis must be excluded on clinical grounds. Performing an arthrocentesis with the goal of obtaining synovial fluid to send for analysis is useful for the following purposes:
A large effusion caused by fluid or blood is painful and leads to significant impairment of joint mobility. Removing synovial fluid as a therapeutic modality is useful for the following purposes:
Elbow arthrocentesis has been employed as an initial treatment measure in patients with radial head fractures, however, a Cochrane review did not find sufficient evidence to permit determination of the effectiveness or safety of this procedure in adults.[6]
Arthrocentesis through overlying cellulitis is controversial because of the concern of seeding the joint with bacteria. This decision should be made in consultation with an orthopedist and with consideration of the potential risks and benefits.
Relative contraindications for elbow arthrocentesis include the following[7] :
The synovial membrane contains pain fibers; therefore, customary practice is to instill a local anesthetic before the procedure to minimize pain. (See Local Anesthetic Agents, Infiltrative Administration.) Typically, lidocaine 1% is used. After the skin is prepared with a povidone-iodine solution or chlorhexidine, make a small wheal with a small (25-gauge) needle in the dermis at the determined entry point for aspiration. Do not inject anesthetic into the joint, because this may hinder synovial fluid analysis.
Alternatively, a topical vapor coolant, such as ethyl chloride, may be sprayed on the skin before needle aspiration. Infrequently, procedural sedation may be required in young children or uncooperative patients.
Equipment used for elbow arthrocentesis includes the following:
Place the patient sitting upright on a stretcher. Bend the patient’s elbow to 90 º. Pronate the patient’s forearm and rest it with the palm down on a side table set at the appropriate height for comfort.
Explain the procedure to the patient and obtain informed consent.
With the patient positioned as described (see Positioning), identify the olecranon process, lateral epicondyle, and radial head, and find the depression (or bulge, if the effusion is large) in the soft triangle. This site is used for all approaches.[8] (See the image below.) Identify the site of entry, and mark the site with a plastic needle sheath or sterile marker. Prepare the skin with a cleansing agent and drape with towels.
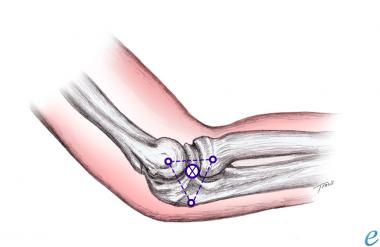 Triangle formed between olecranon, lateral epicondyle, and radial head as site for needle placement.
Triangle formed between olecranon, lateral epicondyle, and radial head as site for needle placement.
Anesthetize the area by injecting 1-2 mL of lidocaine 1% and forming a skin wheal. Insert an 18-gauge needle into the depression perpendicular to both the skin and radial head from the lateral side. This is the lateral approach, which is preferred.
Alternatively, the posterolateral approach can be used. An increased risk of injury to the radial nerve and triceps tendon exists, but this approach is useful if the bulge of an effusion is palpated inferior to the lateral epicondyle. In the posterolateral approach, insert the needle perpendicular to the skin but parallel to the radial shaft. (See the image below.)
 Aspiration of elbow via posterolateral approach.
Aspiration of elbow via posterolateral approach.
Ultrasonography may aid detection of even a small effusion in the olecranon fossa.[9, 10]
Advance the needle slowly while aspirating the syringe until synovial fluid is obtained. If the aspiration is unsuccessful, draw back, reidentify the landmarks, and correct the needle insertion position. If bone is encountered, withdraw the needle slightly and redirect it.
When synovial fluid is obtained, remove the needle Apply a bandage and elastic wrap if a large effusion was present. Place the fluid in specimen tubes and send for analysis.
Do not confuse an olecranon bursitis with a joint effusion. An olecranon bursitis is located posteriorly over the olecranon.
Do not pass the needle through a site with cutaneous signs of infection unless the source is strongly suspected to be from the joint. This should only be done after consultation with an orthopedist.
The landmarks may be easier to find if the arm is first extended to locate the depression and then flexed and pronated for the procedure.
A medial approach should not be used because of risk of injury to the ulnar nerve and the superior ulnar collateral artery.
Arthrocentesis of the elbow or any joint is associated with infrequent complications, including the following:
Copyright © www.orthopaedics.win Bone Health All Rights Reserved