A person with
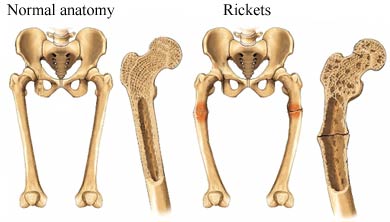
Osteomalacia is said to have “soft bones”. This condition occurs when there is a mineral deficiency or dysfunction in the bone protein matrix known as the osteoid. Primarily composed of collagen, when the osteoid fails to mineralize, the bone's growth plates start to thicken, as well as grow broadly and unevenly.
The lack of vitamin D, and secondarily calcium and phosphorus, coupled with the inability of the body to metabolize these substances, leads to this type of defect in the bone mineralization. The bones become soft due to a calcium deficiency.
Adults have a milder form of the disease called Osteomalacia. It can occur in all age groups, with hereditary Osteomalacia manifesting itself as rickets in children.
OSTEOMALACIA SIGNS AND SYMPTOMS
Osteomalacia most commonly occurs in adults who are dark-skinned or have an unbalanced diet. In most cases,
Osteomalacia shares many of the symptoms of the bone degenerative disease osteoporosis, except that the former is caused by a mineralization defect in the bone's osteoid, its main protein framework, which results from a vitamin D deficiency.
During the early stages of the disease, Osteomalacia is asymptomatic, although x-rays and other related diagnostic tests might show evidence of the disease. The
first symptoms manifest themselves as bone pain, particularly as pain or aching in the lower back and thighs. This bone pain usually spreads out towards the arms and ribs.
Most sufferers describe the pain as symmetrical and non-radiating, often coupled with a sensation of bone tenderness. The muscles surrounding the affected bones also exhibit weakness, and normal activities such as climbing stairs or standing up from a squatting position become more difficult. Generally, the patient will feel weak and fragile, as well as some aches.
As the disease progress, most physical activity becomes uncomfortable, and it is oftentimes accompanied by pain. Patients will notice that gentle pressure on the affected bones can cause severe pain, as well. Muscle weakness and stiffness in the limbs worsen, and any movement will be a cause for discomfort. Most people who are stricken with Osteomalacia can be distinguished by their slow waddling gait.
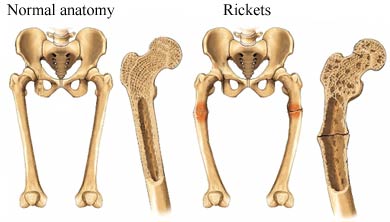 Image: Osteomalacia
Image: Osteomalacia
OSTEOMALACIA DIAGNOSIS
The deformed bones fail to regain their shape in
patients diagnosed with Osteomalacia. In more advanced cases, pathologic fractures become more common as the bones become more and more fragile. Chronic fatigue becomes a constant companion for sufferers, and the low calcium levels cause numbness in the mouth and extremities, spasms in the hands and feet, and arrhythmia.
Vitamin D deficiency is the most common culprit of Osteomalacia. Since this vitamin is primarily responsible for the absorption of calcium, which is the main component of bone building, the lack of Vitamin D results in poor absorption of calcium and other necessary minerals. This malabsorption is the cause of a patient's “soft bones”.
A Vitamin D deficiency in the body usually stems from lack of exposure to the sun. Sunlight is one of the necessary ingredients for the production of Vitamin D in the skin, and Osteomalacia is a common disease in people who get very little sunlight, live in areas where daylight is short or a lot of smog is present, wear a highly potent sunscreen daily, and cover up completely each time they go outdoors. People whose diet is low in Vitamin D-rich foods, such as milk and cereals, or those who fail to take the average daily requirement of Vitamin D in the form of supplements are also prone to Osteomalacia.
In some cases, gastrectomy, a surgical procedure that involves removing a portion or all of a person's stomach, removes a person's ability to metabolize Vitamin D through the gastronomical tract, which in turn need to be absorbed by the intestines. The absence of the small intestines or a major part of the stomach can lead to Osteomalacia.
OSTEOMALACIA CAUSES
Other causes include the autoimmune disorder known as Celiac sprue, where a person's small intestine lining is damaged by gluten-rich food and fail to absorb nutrients; Chronic pancreatitis, when the pancreas becomes inflamed and fails to break down food and nutrients; disorders like kidney failure or primary biliary cirrhosis which interfere with the metabolism of Vitamin D; intake of anti-seizure drugs like phenytoin or phenobarbital, and inherited genetic disorders in which a person has low enzyme levels that are needed to form bones.
To make an accurate diagnosis, the doctor will take down a person's medical history as well as list down the symptoms experienced by the patient. Diet considerations and the amount of sunlight exposure will likewise be determined.
The doctor may order blood and urine tests to check Vitamin D, phosphorous, and calcium levels, x-rays to find any visible cracks in a patient's bones known as Looser transformation zones, bone scans to determine bone metabolism, and even a bone biopsy, to accurately confirm the presence of Osteomalacia.
To rule out any underlying disorder that may be causing the symptoms, the doctor may also recommend PTH tests, Calcium ionized tests, and ALP isoenzyme tests.
OSTEOMALACIA TREATMENT
Treating Osteomalacia will depend on the factors that cause the disease. If Osteomalacia stems from a Vitamin D deficiency, treatment may be composed of increased sunlight exposure, a diet rich in foods containing Vitamin D, and daily supplements of this vitamin, as well as calcium. In some cases, an injection of Vitamin D may be given intravenously.
Patients who exhibit a marked intestinal malabsorption of this vitamin will need larger doses of calcium and Vitamin D. In patients whose Osteomalacia is severe, there are cases when orthopaedic surgery may be necessary. Children with X-lined hypophosphatemic rickets are given supplements rich in calcitrol and phosphate, as well as subject to regular medical monitoring of their condition.
When
Osteomalacia is diagnosed to be secondary to other diseases such as primary biliary cirrhosis or kidney failure, treating the underlying disorder will alleviate Osteomalacia symptoms.
All patients who undergo
treatment for Osteromalacia will likewise undergo regular monitoring to check their phosphorus and calcium levels, as well as take Vitamin D on a regular basis to prevent recurrence of the disease.