

 Rheumatologists are likely to underestimate the impact of osteoarthritis compared to rheumatoid arthritis even though the severity of the conditions can be similar. This is according to a study presented to the Annual Congress of the European League Against Rheumatism.
Rheumatologists are likely to underestimate the impact of osteoarthritis compared to rheumatoid arthritis even though the severity of the conditions can be similar. This is according to a study presented to the Annual Congress of the European League Against Rheumatism.
The authors of the study point out that underestimating the impact of a disease can impact the decisions about choice of therapy. Naturally, treatment can, in turn, impact outcome.
In the past, studies on rheumatic ailments, including rheumatoid arthritis, showed that doctors and patients rate the impact of the disease very differently. Recent data shows that both rheumatoid arthritis and osteoarthritis have similar burdens, but osteoarthritis is usually considered less severe than rheumatoid arthritis or as many call it, RA.
In this latest study, patient perception of the ailment severity was greater than physician assessment in one third of osteoarthritis patients and one fifth of RA patients. In just one half of osteoarthritis and two thirds of RA patients, the assessments were equivalent. Assessment is based on a scale of 0 to 10. Patient assessment involved completing a questionnaire that included scores for physical function, pain, fatigue, and other symptoms, as well as a joint report.
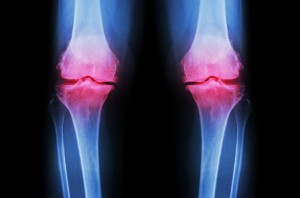
Both osteoarthritis and RA involve joint pain and a decrease in range of motion, but make no mistake, there is a difference between osteoarthritis and rheumatoid arthritis that people have to take into account.
Often called degenerative joint disease, osteoarthritis is one of the most common chronic conditions of the joints. It affects about 27 million Americans. While osteoarthritis can affect any joint, it occurs most often in the hips, knees, neck, and lower back. It can also impact the small joints of the fingers and the bases of the thumb and big toe.
Rheumatoid arthritis is an autoimmune disorder that takes place when your immune system attacks your own tissues. Unlike the wear-and-tear of osteoarthritis, RA impacts the lining of your joints, leading to swelling that can cause bone erosion and joint deformity.
While the two diseases share some symptoms, there are some signs that differ. For example, joint stiffness and pain are common in both osteoarthritis and RA, but people who suffer from RA also experience swelling, fatigue, and in some cases, fever. The location of the pain is also different. In osteoarthritis sufferers, the pain tends to be in the weight-bearing joints, such as the knees, hip, and neck, while for RA sufferers it is more likely to be in joint pairs, like the hands or ankles. There is also a slight variation in when pain occurs. When a person has osteoarthritis, pain tends to worsen after a day of activity, but with rheumatoid arthritis patients, the pain can be worse in the morning or at night at the end of a long day of activity.
Many people have wondered, can you have osteoarthritis and rheumatoid arthritis at the same time? The answer is yes, you can have both osteoarthritis and RA. For instance, you may have a knee affected by rheumatoid arthritis, but your spine can have degenerative changes that are due to a diagnosis of osteoarthritis.
Osteoarthritis and rheumatoid arthritis are two of the most common causes of disability in America. These conditions have a significant impact on the workforce, on family life, and on our healthcare system. Early diagnosis and treatment to help treat the symptoms and slow down the progression of the diseases is key to maintaining a more productive life.
Copyright © www.orthopaedics.win Bone Health All Rights Reserved